Mastering Experimental Design for Source of Variation Analysis: A Strategic Guide for Researchers
This article provides a comprehensive framework for researchers and drug development professionals to design robust experiments that effectively identify, quantify, and control sources of variation.
Mastering Experimental Design for Source of Variation Analysis: A Strategic Guide for Researchers
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to design robust experiments that effectively identify, quantify, and control sources of variation. Covering foundational concepts to advanced applications, it explores methodological approaches like Design of Experiments (DoE) and variance component analysis, troubleshooting strategies for common pitfalls, and validation techniques for comparative studies. The guide synthesizes principles from omics research, pharmaceutical development, and clinical trials to empower scientists in building quality into their research, minimizing bias, and drawing reliable, reproducible conclusions from complex data.
Laying the Groundwork: Core Principles for Identifying Sources of Variation
Frequently Asked Questions
What are the major sources of variability in biological experiments? The hierarchy of variability spans from molecular differences between individual cells to significant differences between patients. The greatest source of variability often comes from biological factors such as tissue heterogeneity (different regions of the same biopsy) and inter-patient variation, rather than technical experimental error [1]. Even in relatively homogeneous tissues like muscle, different biopsy regions show substantial variation in cell type content [1].
Why do my cultured cell results not translate to primary tissues? Cultured cells exhibit fundamentally different biology from primary tissues. Lipidomic studies reveal that primary membranes (e.g., erythrocytes, synaptosomes) sharply diverge from all cultured cell lines, with primary tissues containing more than double the abundance of highly unsaturated phospholipids [2]. This "unnatural" lipid composition in cultured cells is likely driven by standard culture media formulations lacking polyunsaturated fatty acids [2].
How can I minimize variability in expression profiling studies? Pre-profile mixing of patient samples can effectively normalize both intra- and inter-patient sources of variation while retaining profiling specificity [1]. One study found that experimental error (RNA, cDNA, cRNA, or GeneChip) was minor compared to biological variability, with mixed samples maintaining 85-86% of statistically significant differences detected by individual profiles [1].
How do I troubleshoot failed PCR experiments? Follow a systematic approach: First, identify the specific problem (e.g., no PCR product). List all possible causes including each master mix ingredient, equipment, and procedure. Collect data by checking controls, storage conditions, and your documented procedure. Eliminate unlikely explanations, then design experiments to test remaining possibilities [3].
What should I do when no clones grow on my transformation plates? Check your control plates first. If colonies grow on controls, the problem likely lies with your plasmid, antibiotic, or transformation procedure. Systematically test your competent cell efficiency, antibiotic selection, heat shock temperature, and finally analyze your plasmid DNA for integrity and concentration [3].
Troubleshooting Guides
Guide 1: Systematic Troubleshooting for Failed Experiments
Problem Identification
- Define the specific failure: Precisely note what went wrong without assuming causes [3]
- Check controls first: Determine if positive/negative controls worked as expected [3]
- Document everything: Record all observations in your laboratory notebook [4]
Root Cause Analysis
Implementation and Verification
- Design targeted experiments to test remaining hypotheses [3]
- Change one variable at a time while keeping others constant [4]
- Verify the solution by reproducing results multiple times [4]
- Document the resolution for future reference [3]
Guide 2: Addressing Cell Line vs. Primary Tissue Discrepancies
Recognizing the Limitations of Cultured Cells
Table 1: Key Lipidomic Differences Between Cultured Cells and Primary Tissues
| Lipid Characteristic | Cultured Cells | Primary Tissues | Functional Significance |
|---|---|---|---|
| Polyunsaturated Lipids | Low abundance (<10%) | High abundance (>20%) | Membrane fluidity, signaling |
| Mono/Di-unsaturated Lipids | High abundance | Lower abundance | Membrane physical properties |
| Plasmenyl Phosphatidylcholine | Relatively abundant | Scarce in primary samples | Oxidative protection |
| Sphingomyelin Content | Variable | Tissue-specific enrichment | Membrane microdomains |
Experimental Strategies to Bridge the Gap
- Supplement culture media with polyunsaturated fatty acids to better recapitulate in vivo conditions [2]
- Validate key findings in multiple model systems including primary cells [2]
- Consider tissue-specific lipidomics when designing drug delivery systems [2]
- Account for donor variability by using multiple primary sources [1]
Guide 3: Managing Variability in Expression Profiling
Understanding Variability Sources
Table 2: Relative Contribution of Different Variability Sources in Expression Profiling
| Variability Source | Relative Impact | Management Strategy |
|---|---|---|
| Tissue Heterogeneity (different biopsy regions) | Highest | Sample mixing, multiple biopsies |
| Inter-patient Variation (SNP noise) | High | Larger sample sizes, careful matching |
| Experimental Procedure (RNA/cRNA production) | Moderate | Standardized protocols, quality control |
| Microarray Hybridization | Low | Technical replicates, normalization |
Protocol: Sample Mixing for Variability Normalization
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Variability Analysis
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Shotgun Lipidomics (ESI-MS/MS) | Comprehensive lipid profiling | Measures 400-800 individual lipid species per sample; reveals membrane composition differences [2] |
| Principal Component Analysis (PCA) | Dimensionality reduction for complex datasets | Identifies major sources of variation; compresses lipidomic variation into interpretable components [2] |
| Affymetrix GeneChips | Expression profiling platform | Provides standardized, redundant oligonucleotide arrays for transportable data [1] |
| Premade Master Mixes | PCR reaction consistency | Reduces experimental error compared to homemade mixes [3] |
| Quality Controlled Competent Cells | Reliable transformation | Maintain transformation efficiency for at least one year with proper storage [3] |
Advanced Technical Notes
Protocol: Shotgun Lipidomics for Membrane Variability Analysis
Sample Preparation
- Isolate membranes using standardized protocols (plasma membrane vs. whole cell membranes)
- Extract lipids maintaining consistency across samples
- Include quality controls from reference materials
ESI-MS/MS Analysis
- Utilize electrospray ionization tandem mass spectrometry
- Quantify 400-800 individual lipid species per sample
- Measure abundance from 0.001 mol% to 40 mol% (cholesterol)
Data Interpretation
- Perform PCA to identify major sources of variation
- Analyze both phospholipid headgroups and total lipid unsaturation
- Compare loadings to understand segregating features [2]
Protocol: Managing Inter-patient Variability in Human Studies
Experimental Design
- Collect multiple biopsies from each patient when possible
- Process RNAs individually initially
- Use mixing strategies to normalize SNP noise
- Maintain strict quality control criteria
Quality Control Parameters
- Sufficient cRNA amplification
- Post-hybridization scaling factors (ideal range: 0.5-3.0)
- Percentage present calls consistency
- Correlation coefficients between replicates [1]
Frequently Asked Questions
1. What is the fundamental difference between a biological and a technical replicate?
A biological replicate is a distinct, independent biological sample (e.g., different mice, independently grown cell cultures, or different human patients) that captures the random biological variation found in the population or system under study. In contrast, a technical replicate is a repeated measurement of the same biological sample. It helps quantify the variability introduced by your measurement technique itself, such as pipetting error or instrument noise [5] [6].
2. What is pseudoreplication and why is it a problem?
Pseudoreplication occurs when technical replicates are mistakenly treated as if they were independent biological replicates [6]. This is a serious error because it artificially inflates your sample size in statistical analyses. Treating non-independent measurements as independent increases the likelihood of false positive results (Type I errors), leading you to believe an experimental effect is real when it may not be [6].
3. How many technical replicates are optimal for evaluating my measurement system?
For experiments designed to evaluate the reproducibility or reliability of your measurements (often called "Type B" experiments), the optimal allocation is to use two technical replicates for each biological replicate when the total number of measurements is fixed. This configuration minimizes the variance in estimating your measurement error [7].
4. Can I use technical replicates to increase my statistical power for biological questions?
Not directly. Technical replicates primarily help you understand and reduce the impact of measurement noise. For statistical analyses that ask biological questions (e.g., "Does this treatment change gene expression?"), the sample size (n) is the number of biological replicates, not the total number of measurements. To increase power for these "Type A" experiments, you should increase the number of biological replicates [7] [6].
5. My samples are very expensive, but assays are cheap. Can I just run many technical replicates?
While you can, it will not help you generalize your findings. If you use only one biological replicate (e.g., cells from a single donor) with many technical replicates, your conclusions are only valid for that one donor. You cannot know if the results apply to the broader population. A better strategy is to find a balance, perhaps using a moderate number of biological replicates with a smaller number of technical replicates to control measurement error [7].
Troubleshooting Guide: Common Scenarios
| Scenario | Potential Issue | Recommended Solution |
|---|---|---|
| High variability between technical replicates. | Your measurement protocol or instrumentation may be unstable or imprecise [5]. | Review and optimize your assay protocol. Check instrument calibration. Use technical replicates to identify and reduce sources of measurement error. |
| No statistical significance despite large observed effect. | Likely due to too few biological replicates, resulting in low statistical power [6]. | Increase the number of independent biological replicates. Statistical power is driven by the number of biological, not technical, replicates. |
| Statistical analysis shows a significant effect, but the result does not hold up in a follow-up experiment. | Potential pseudoreplication. Treating technical replicates or non-independent samples as biological replicates inflates false positive rates [6]. | Re-analyze your data, ensuring the statistical n matches the number of true biological replicates. Use mixed-effects models if non-independence is inherent to the design. |
| Uncertainty in whether a sample is a true biological replicate. | The definition might be unclear for complex experimental designs (e.g., cells from the same tissue culture flask, pups from the same litter) [6]. | Apply the three criteria for true biological replication: 1) Random assignment to conditions, 2) Independent application of the treatment, and 3) Inability of individuals to affect each other's outcome. |
Experimental Protocols for Proper Replication
Protocol 1: Establishing a Valid Replication Strategy
- Define Your Experimental Unit: Identify the smallest independent entity to which a treatment can be applied. This is your potential biological replicate (e.g., a single mouse, a culture of cells seeded from an independent vial, a separately transfected well).
- Apply Treatments Independently: Ensure that the treatment for one biological replicate does not depend on and is not applied simultaneously with another. For example, treat cells in separate culture vessels with individually prepared drug dilutions rather than adding one concentration to a shared bath.
- Prevent Cross-Influence: House animals or process samples in a way that prevents one from influencing the other. This may require separate caging or independent processing [6].
- Determine Replicate Numbers:
- Biological Replicates: Plan for a sufficient number based on a power analysis. This is the most critical factor for the validity of your biological conclusions.
- Technical Replicates: For assessing measurement reliability, use two per biological sample [7]. For routine experiments, duplicate or triplicate technical measurements can help control for assay-level variability.
Protocol 2: Quantitative Western Blot Analysis with Replicate Samples
This protocol exemplifies how to integrate both replicate types for robust quantification [5].
- Prepare Biological Replicates: Culture and treat cells in at least three independent batches (biological replicates
n=3). - Prepare Technical Replicates: For each biological sample, prepare two or more separate protein lysates (technical replicate 1). Load each lysate onto the same gel or parallel gels (technical replicate 2).
- Image and Quantify: Detect bands and quantify signal intensity.
- Analyze Data: Normalize target protein signal to a validated loading control. First, average the technical replicate measurements for each biological sample. Then, perform statistical comparisons across the means of the independent biological replicates (
n=3).
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Independently Cultured Cell Batches | The foundation of in vitro biological replication. Cells cultured and passaged separately mimic population-level variation. |
| Genetically Distinct Animal Models | Crucial for in vivo biological replication. Using different animals accounts for genetic and physiological variability. |
| Revert 700 Total Protein Stain | A superior normalization method for Western blotting. Stains all proteins, providing a more reliable loading control than a single housekeeping protein [5]. |
| Validated Housekeeping Antibodies | Used for traditional Western blot normalization. Must be validated to confirm their expression is constant across all experimental conditions [5]. |
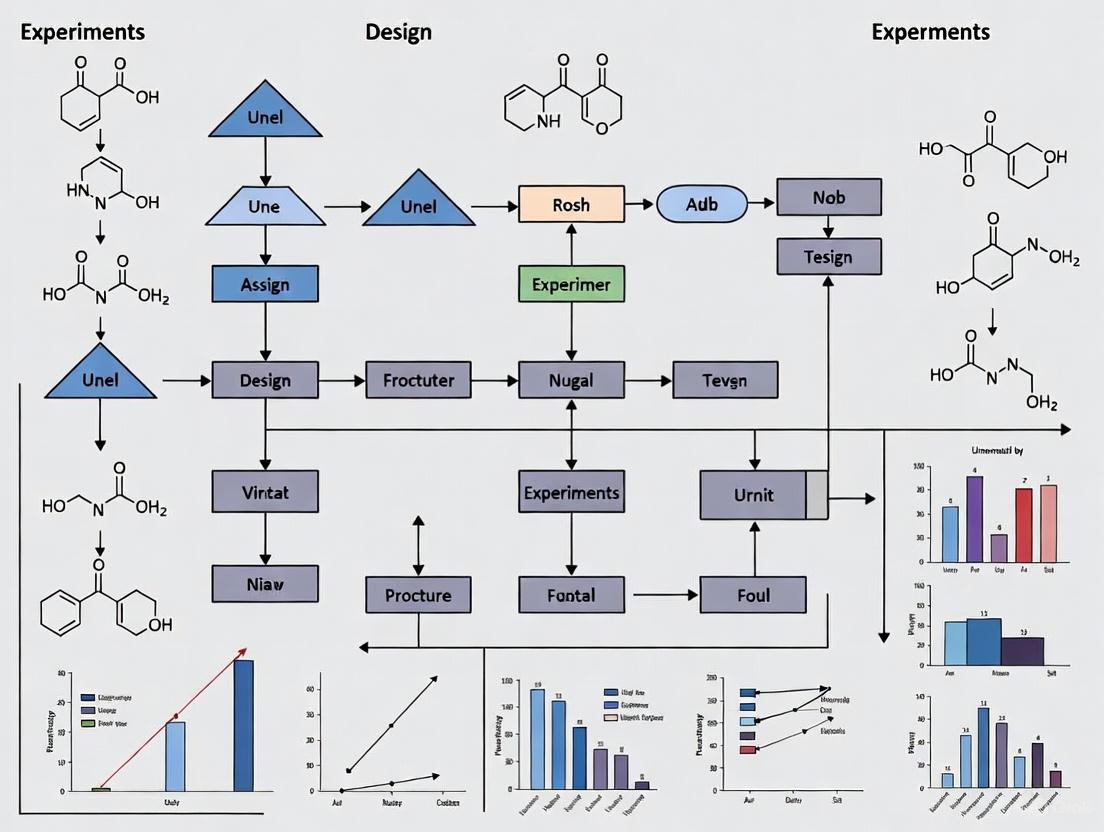
Relationships and Workflow Diagrams
The following diagrams, created using DOT language, illustrate the core concepts and logical relationships in replicate-based experimental design.
Troubleshooting Guides
Troubleshooting Guide 1: Pseudoreplication
What is the problem? Pseudoreplication occurs when data points are not statistically independent but are treated as independent observations in an analysis. This artificially inflates your sample size and invalidates statistical tests [8] [9].
How to diagnose it: Ask these questions about your experimental design:
- Q1: What is the smallest unit to which my treatment is independently applied? This is your true experimental unit [9].
- Q2: Are my "replicates" actually multiple measurements from the same experimental unit? If yes, these are repeated measures or pseudoreplicates, not true replicates [8] [10].
- Q3: Could measurements within a group be more similar to each other due to a shared source? This hierarchical structure (e.g., cells within an animal, plants within a plot) indicates potential pseudoreplication [10].
Table: Identifying Experimental Units and Pseudoreplicates
| Experimental Scenario | True Experimental Unit | Common Pseudoreplicate | Why It's a Problem |
|---|---|---|---|
| Testing a drug on 5 rats, measuring each 3 times [8] | The rat | The 3 measurements per rat | Measurements from one rat are not independent; analysis must account for the "rat" effect. |
| Growing plants in 2 chambers with different CO₂, 5 plants per chamber [9] | The growth chamber | The individual plants in a chamber | All plants in one chamber share the same environment; treatment effect is confounded with chamber effect. |
| Comparing two curricula in two schools, testing all students [9] | The school | The individual students | Student results are influenced by teacher and school factors; you only have one replicate per treatment. |
| Single-cell RNA-seq from 3 individuals, 100s of cells per individual [10] | The individual person | The individual cells | Cells from the same person share a genetic and environmental background and are not independent. |
How to fix it:
- Design Phase: Ensure your treatment is applied to multiple, independent experimental units [9].
- Analysis Phase: Use statistical models that account for the non-independent structure of your data:
- Mixed-effects models include a random effect for the grouping variable (e.g.,
Rat_ID,Patient_ID,Growth_Chamber) to account for the correlation within groups [10]. - Aggregation methods (e.g., pseudo-bulk) involve averaging the values within each experimental unit first, then performing the analysis on those unit-level means [10].
- Mixed-effects models include a random effect for the grouping variable (e.g.,
The diagram below illustrates the correct way to model data with a hierarchical structure to avoid pseudoreplication.
Troubleshooting Guide 2: Confounding
What is the problem? Confounding occurs when the apparent effect of your treatment of interest is mixed up with the effect of a third, "confounding" variable. This makes it impossible to establish a true cause-and-effect relationship [11] [9].
How to diagnose it: A confounding variable must meet all three of these criteria:
- It is a cause (or a good proxy for a cause) of the outcome.
- It is associated with the treatment or exposure of interest.
- It is not an intermediate step in the causal pathway between the treatment and the outcome [11].
Table: Confounding in Experimental Design
| Scenario | Treatment of Interest | Outcome | Potential Confounder | Why It Confounds |
|---|---|---|---|---|
| Observational study | Coffee drinking | Lung cancer | Smoking | Smoking causes lung cancer and is associated with coffee drinking. |
| Growth chamber experiment [9] | CO₂ level | Plant growth | Growth chamber | Chamber-specific conditions (light, humidity) affect growth and are perfectly tied to the CO₂ treatment. |
| Drug efficacy study | New Drug vs. Old Drug | Patient recovery | Disease severity | If sicker patients are given the new drug, its effect is confounded by the initial severity. |
How to fix it:
- Randomization: Randomly assign your experimental units to treatment groups. This helps ensure that potential confounders are distributed evenly across groups [11].
- Restriction: Only include subjects within a specific category of the confounder (e.g., only studying 50-60 year-olds to control for age).
- Statistical Control: In your analysis, include the confounding variable as a covariate in a regression model. Caution: Avoid the "Table 2 Fallacy" of interpreting the coefficients of the confounders as causal [11].
Troubleshooting Guide 3: Underpowered Studies
What is the problem? An underpowered study has a sample size that is too small to reliably detect a true effect of the magnitude you are interested in. This leads to imprecise estimates and a high probability of falsely concluding an effect does not exist (Type II error) [11].
How to diagnose it: Your study is likely underpowered if:
- You used a "rule of thumb" for sample size instead of a formal power calculation [11].
- Your confidence intervals for the primary effect are very wide.
- You find a non-significant result (p > 0.05) but the point estimate of the effect is large enough to be scientifically interesting.
Table: Impact of Sample Size and Pseudoreplication on Power and Error
| Condition | Statistical Power | Type I Error (False Positive) Rate | Precision of Effect Size Estimate |
|---|---|---|---|
| Appropriate sample size, independent data | Adequate | Properly controlled (e.g., 5%) | Accurate |
| Too few experimental units (Underpowered) | Low | Properly controlled | Low, confidence intervals are wide |
| Pseudoreplication (e.g., analyzing cells, not people) | Inflated (falsely high) | Dramatically inflated [8] [10] [12] | Overly precise, confidence intervals are falsely narrow [8] |
How to fix it:
- A Priori Power Analysis: Before collecting data, conduct a sample size calculation. This requires you to specify:
- The expected effect size (based on pilot data or literature).
- The desired statistical power (typically 80% or 90%).
- The alpha level (typically 0.05).
- Focus on the Experimental Unit: Ensure your power calculation is based on the number of independent experimental units (e.g., the number of animals or human participants), not the number of technical measurements or pseudoreplicates [12].
- Precision Analysis: Alternatively, you can calculate the sample size needed to achieve a desired confidence interval width for your effect estimate.
Frequently Asked Questions (FAQs)
Q1: My field commonly uses "n" to represent the number of cells/technical replicates. Is this pseudoreplication? Yes, this is a very common form of pseudoreplication. The sample size (n) should reflect the number of independent experimental units (e.g., individual animals, human participants, independently treated culture plates) [8] [10]. Measurements nested within these units (cells, technical repeats) are subsamples or pseudoreplicates. Reporting the degrees of freedom (df) for statistical tests can help reveal this error, as the df should be based on the number of independent units [8].
Q2: I have a balanced design with the same number of cells per patient. Can't I just average the values and do a t-test? Yes, this aggregation approach (creating a "pseudo-bulk" value for each patient) is a valid and conservative method to avoid pseudoreplication [10]. However, it can be underpowered, especially if the number of cells per individual is imbalanced. A more powerful and statistically rigorous approach is to use a mixed model with a random effect for the patient, which explicitly models the within-patient correlation [10].
Q3: I corrected for "batch" in my analysis. Does this solve pseudoreplication? No, not necessarily. A standard batch effect correction (like ComBat) is not designed to handle the specific correlation structure of pseudoreplicated data. In fact, simulations have shown that applying batch correction prior to differential expression analysis can further inflate type I error rates [10]. The recommended solution is to use a model with a random effect for the experimental unit (e.g., individual).
Q4: How widespread is the problem of pseudoreplication? Alarmingly common. A 2025 study found that pseudoreplication was present in the majority of rodent-model neuroscience publications examined, and its prevalence has increased over time despite improvements in statistical reporting [12]. An earlier analysis of a single neuroscience journal issue found that 12% of papers had clear pseudoreplication, and a further 36% were suspected of it [8].
The Scientist's Toolkit
Table: Essential Reagents for Robust Experimental Design
| Tool or Method | Function | Key Consideration |
|---|---|---|
| A Priori Power Analysis | Calculates the required number of independent experimental units to detect a specified effect size, preventing underpowered studies [11]. | Requires an estimate of the expected effect size from pilot data or literature. |
| Generalized Linear Mixed Models (GLMM) | Statistical models that properly account for non-independent data (pseudoreplication) by including fixed effects for treatments and random effects for grouping factors (e.g., Individual, Litter) [10]. | Computationally intensive and requires careful model specification. Ideal for single-cell or repeated measures data. |
| Randomization Protocol | A procedure for randomly assigning experimental units to treatment groups to minimize confounding and ensure that other variables are evenly distributed across groups. | The cornerstone of a causal inference study. Does not eliminate confounding but makes it less likely. |
| Blocking | A design technique where experimental units are grouped into blocks (e.g., by age, sex, batch) to control for known sources of variation before random assignment. | Increases precision and power by accounting for a known nuisance variable. |
Defining Your Experimental Unit and Unit of Randomization
Frequently Asked Questions
What is an experimental unit? An experimental unit is the smallest division of experimental material such that any two units can receive different treatments. It is the primary physical entity (a person, an animal, a plot of land, a dish of cells) that is the subject of the experiment and to which a treatment is independently applied [13] [14]. In a study designed to determine the effect of exercise programs on patient cholesterol levels, each patient is an experimental unit [14].
What is a unit of randomization? The unit of randomization is the entity that is randomly assigned to a treatment group. Randomization is the process of allocating these units to the investigational and control arms by chance to prevent systematic differences between groups and to produce comparable groups with respect to both known and unknown factors [15].
Are the experimental unit and the unit of randomization always the same? Not always. The experimental unit is defined by what receives the treatment, while the unit of randomization is defined by how treatments are assigned. While they are often the same entity, in more complex experimental designs, they can differ [16]. The key is that randomization must be applied at the level of the experimental unit, or a level above it, to ensure valid statistical comparisons [17].
What happens if I misidentify the experimental unit? Misidentifying the experimental unit is a critical error that can lead to pseudoreplication—where multiple non-independent measurements are mistakenly treated as independent replicates [17]. This inflates the apparent sample size, invalidates the assumptions of standard statistical tests, and can lead to unreliable conclusions and wasted resources [13] [17].
What are common sources of randomization errors in clinical trials? Several common issues can occur [18] [15]:
- Randomizing an ineligible participant.
- Selecting the wrong stratification group for a participant.
- Randomizing a participant before all eligibility criteria are confirmed.
- A single participant being randomized multiple times.
- Dispensing the incorrect drug kit to a randomized participant.
Troubleshooting Guides
Problem: I'm unsure how to identify the experimental unit in my study.
Guide: A Step-by-Step Method for Identification Follow this logical process to correctly identify your experimental unit.
Verification Protocol: Once you have a candidate for your experimental unit, ask these questions to verify your choice [19] [17]:
- Question of Independence: Is the treatment applied to this unit independent of the treatment applied to all other units? If the treatment application to one unit potentially affects another, your experimental unit is likely a larger grouping (e.g., the cage of animals, not the individual animal).
- Question of Replication: Does counting this entity give you the true number of independent data points (replicates) for your treatment? If you are taking multiple measurements from the same entity (e.g., three leaf samples from one plant), those are subsamples, not experimental units. The plant itself is the experimental unit.
Real-World Contextual Examples:
- Clinical Trial: Testing a new drug. The experimental unit is the individual patient [14].
- Agriculture: Testing fertilizers. The experimental unit is the plot of land that receives one type of fertilizer, even if you measure multiple plants within that plot.
- Manufacturing: Testing a new menu item in a restaurant chain. The experimental unit is the restaurant, not the individual sandwich or customer, as the intervention is applied at the restaurant level [17].
- Preclinical Animal Study: Testing diet and vitamin supplements. The experimental unit for the diet might be the entire cage of mice (if all mice in a cage eat the same diet), while the experimental unit for the vitamin supplement could be the individual mouse (if each mouse is independently supplemented) [17].
Problem: A randomization error has occurred in my trial.
Guide: Responding to Common Randomization Errors Adhering to the Intention-to-Treat (ITT) principle is crucial when handling errors. The ITT principle states that all randomized participants should be analyzed in their initially randomized group to maintain the balance achieved by randomization and avoid bias [18]. The general recommendation is to document errors thoroughly, not to attempt to "correct" or "undo" them after the fact, as corrections can introduce further issues and bias [18].
The table below summarizes guidance for specific error types based on established clinical trial practice [18].
| Error Type | Recommended Action | Rationale |
|---|---|---|
| Ineligible Participant Randomized | Keep the participant in the trial; collect all data. Seek clinical input for management. Only exclude if a pre-specified, unbiased process exists. | Maintaining the initial randomization preserves the integrity of the group comparison and prevents selection bias [18]. |
| Participant Randomized with Incorrect Baseline Info | Accept the randomization. Record the correct baseline information in the dataset. | The allocation is preserved for analysis, while accurate baseline data allows for proper characterization of the study population [18]. |
| Multiple Randomizations for One Participant | Scenario A: Only one set of data will be obtained → Retain the first randomization. Scenario B: Multiple data sets will be obtained → Retain both randomizations. | This provides a consistent, unbiased rule that maintains the randomized cohort for analysis [18]. |
| Incorrect Treatment Dispensed | Document the treatment the participant actually received. Seek clinical input regarding their ongoing care. For analysis, the participant remains in their originally randomized group (ITT) but can be excluded from the per-protocol sensitivity analysis [18] [15]. | This documents reality without altering the original randomized group structure, which is essential for the primary analysis [18]. |
The Scientist's Toolkit: Essential Reagents for Robust Design
| Tool or Reagent | Function in Experimental Design |
|---|---|
| Interactive Response Technology (IRT) | An automated system (phone or web-based) for managing random assignment of treatments and drug inventory in clinical trials, which helps minimize bias and errors [15]. |
| Stratified Randomization | A technique to ensure treatment groups are balanced with respect to specific, known baseline variables (e.g., disease severity, age group) that strongly influence the outcome [18] [15]. |
| Blocking (Randomized Block Design) | A design principle where experimental units are grouped into "blocks" based on a shared characteristic (e.g., a litter of mice, a batch of reagent). Treatments are then randomized within each block, accounting for a known source of variability [20]. |
| Intention-to-Treat (ITT) Principle | The gold-standard analytical approach where all participants are analyzed in the group to which they were originally randomized, regardless of protocol deviations, errors, or non-compliance. It preserves the benefits of randomization [18]. |
| Experimental Design Assistant (EDA) | A tool to help researchers visually map out the relationships in their experiment, including interventions and experimental units, to ensure clarity and correct structure before the experiment begins [17]. |
Protocol: Implementing a Randomized Block Design
This protocol is essential when a known source of variation (e.g., clinical site, technician, manufacturing batch) could confound your results.
Objective: To control for a nuisance variable by grouping experimental units into homogeneous blocks and randomizing treatments within each block.
Methodology:
- Identify the Blocking Factor: Determine the variable that creates significant, unwanted variation (e.g., "clinical site," "day of the week," "baseline severity score").
- Form Blocks: Group your experimental units into blocks based on this factor. Each block should contain units that are as similar as possible to each other. The number of units per block must be a multiple of the number of treatments.
- Randomize Within Blocks: Independently randomize the assignment of treatments to the experimental units within each block. For example, if you have two treatments (A and B) and a block of 4 units, you would randomly assign 2 units to A and 2 to B within that block.
- Execute Experiment: Apply the treatments and collect data according to the randomized assignment.
- Analyze Data: Use a statistical model (e.g., ANOVA for blocked designs) that includes both the treatment effect and the block effect. This model separates the variation due to the blocking factor from the variation due to the treatment, giving a more precise estimate of the treatment effect.
Troubleshooting Guides
Fundamental Guide: My Experiment Shows No Signal or Effect
Problem: You run your experiment, but the results show no change or signal, even in the experimental group where an effect is expected.
Diagnosis Approach: This problem suggests that your experimental system is not functioning or detecting the phenomenon. Your primary goal is to verify that your test is working correctly.
Solution:
- Implement a Positive Control: Introduce a treatment or sample known to produce a positive result [21] [22]. For example, if testing a new drug, use a known effective drug as a positive control.
- Interpretation:
- If the positive control works: Your experimental system is functional. The lack of effect in your experimental group is likely a true negative result, or your treatment is ineffective at the tested concentration/dose.
- If the positive control fails: Your experimental method, reagents, or equipment are faulty. The problem is with your assay, not necessarily your experimental variable.
Recommended Actions Table:
| Action | Purpose | Example |
|---|---|---|
| Run a positive control | Verifies the experimental system can detect a positive signal [21]. | In a PCR, use a template known to amplify. |
| Check reagent integrity | Confirms reagents are active and not degraded. | Check expiration dates; prepare fresh solutions. |
| Verify equipment function | Ensures instruments are calibrated and working [21]. | Run a calibration standard on a spectrophotometer. |
| Re-test with a wider concentration range | Rules out that the effect occurs at a different concentration. | Test additional doses of a compound. |
Intermediate Guide: My Negative Control is Showing a Positive Result
Problem: Your negative control, which should not produce an effect, is showing a signal or change. This indicates a potential false positive in your experiment.
Diagnosis Approach: A signal in the negative control suggests that your results are not solely due to your experimental variable. Your goal is to identify and eliminate the source of this contamination or non-specific signal [21] [23].
Solution:
- Systematic Elimination: Investigate common sources of contamination or interference.
- Interpretation: The specific result of your checks will point you toward the root cause.
Troubleshooting Flowchart:
Advanced Guide: My Results Have High, Unexplained Variability
Problem: Your experimental data shows high error bars or significant variability between replicates, making it difficult to draw clear conclusions about the source of variation.
Diagnosis Approach: High variability obscures the true effect of your experimental variable. You must identify and control for the unintended sources of variation (nuisance variables).
Solution:
- Analyze Your Experimental Design: Move away from a One-Factor-at-a-Time (OFAT) approach, which can miss interactions between factors and is inefficient for finding optimal conditions [24].
- Implement a Designed Experiment (DOE): Use a systematic approach like Design of Experiments (DOE) to efficiently study the effects of multiple factors and their interactions on your response variable [24].
- Review Technical Execution: High variability often stems from inconsistencies in technique, as demonstrated in a cell viability assay where careful pipetting during wash steps was critical to reducing variance [23].
DOE vs. OFAT Comparison Table:
| Aspect | One-Factor-at-a-Time (OFAT) | Design of Experiments (DOE) |
|---|---|---|
| Efficiency | Low; requires many runs to test multiple factors [24]. | High; tests multiple factors and interactions simultaneously with fewer runs [24]. |
| Interaction Detection | Cannot detect interactions between factors [24]. | Specifically designed to detect and quantify factor interactions [24]. |
| Optimal Setting | Likely misses the true optimum if factor interactions exist [24]. | Uses a model to predict the true optimal settings within the tested region [24]. |
| Best Use Case | Preliminary, exploratory experiments with a single suspected dominant factor. | Systematically understanding complex systems with multiple potential sources of variation [24]. |
Frequently Asked Questions (FAQs)
Fundamental Concepts
Q1: What is the difference between a control group and an experimental group? The experimental group is exposed to the independent variable (the treatment or condition you are testing). The control group is identical in every way except it is not exposed to the independent variable. This provides a baseline to compare against, ensuring any observed effect is due to the treatment itself and not other factors [22].
Q2: Why are positive and negative controls necessary if I already have a control group? A control group (or experimental control) provides a baseline for a specific experiment. Positive and negative controls are used to validate the experimental method itself [21] [25].
- A positive control ensures your test can produce a positive result, verifying that all reagents and equipment are working [21] [22].
- A negative control ensures your test does not produce a false positive signal due to contamination or non-specific effects [21] [22]. Together, they confirm the validity and reliability of your results.
Q3: Can a control group also be a positive or negative control? Yes. A single group can serve multiple roles. For example, in a drug trial, the group receiving a standard, commercially available medication is both a control group (for comparison to the new drug) and a positive control (to prove the trial can detect a therapeutic effect) [22].
Implementation and Troubleshooting
Q4: How do I choose the right positive control for my experiment? A valid positive control must be a material or condition known to produce the expected outcome through a well-established mechanism. Examples include [21]:
- A known enzyme activator in an enzyme activity assay.
- A proven antimicrobial agent in a disinfectant test.
- A sample confirmed to contain the target analyte in a diagnostic test.
Q5: My positive control failed. What should I do next? A failed positive control indicates a fundamental problem with your experimental setup. Immediately stop testing and investigate the following:
- Reagent Integrity: Check expiration dates, preparation methods, and storage conditions.
- Equipment Function: Verify that instruments are calibrated, powered on, and functioning correctly [21].
- Protocol Execution: Carefully review the procedure for any errors or deviations.
Q6: How can I formally improve my troubleshooting skills? Troubleshooting is a core scientific skill. Structured approaches, such as the "Pipettes and Problem Solving" method used in graduate training, can be highly effective. This involves [23]:
- Scenario Presentation: A leader presents a detailed experiment with unexpected results.
- Collaborative Dialogue: The group asks specific questions about the experimental setup.
- Consensus Experimentation: The group must agree on a limited number of new experiments to diagnose the problem.
- Result Interpretation: The leader provides mock results, guiding the group to the root cause.
The Scientist's Toolkit
Research Reagent Solutions
Essential Materials for Controlled Experimentation
| Reagent/Material | Function in Experimental Controls |
|---|---|
| Placebo | An inert substance (e.g., a sugar pill) used as a negative control in clinical or behavioral studies to account for the placebo effect [22]. |
| Known Actives/Agonists | A compound known to activate the target or pathway. Serves as a critical positive control to demonstrate assay capability [22]. |
| Vehicle Control | The solvent (e.g., DMSO, saline) used to deliver the experimental compound. A negative control to ensure the vehicle itself does not cause an effect. |
| Wild-Type Cell Line/Strain | An unmodified biological system used as a control to compare against genetically modified or treated groups, establishing a baseline phenotype. |
| Housekeeping Gene Antibodies | Antibodies against proteins (e.g., GAPDH, Actin) that are constitutively expressed. Used as a loading control in Western blots to ensure equal protein loading across all samples, including controls. |
Experimental Protocol: Vitamin C Detection Assay
Aim: To determine whether a fruit juice contains Vitamin C. Principle: The blue dye DCPIP is decolorized in the presence of Vitamin C.
Methodology:
- Sample Preparation: Prepare a solution of the fruit juice in distilled water. In a test tube, add a fixed volume of DCPIP solution.
- Titration: Titrate the fruit juice solution into the DCPIP dropwise, with gentle shaking, until the blue color disappears completely. Record the volume of juice used.
- Control Setup:
- Positive Control: Repeat the titration using a known Vitamin C solution (e.g., ascorbic acid of known concentration). This should successfully decolorize DCPIP, confirming the test is working [21].
- Negative Control: Repeat the titration using distilled water. The blue color of DCPIP should not disappear. Any color change indicates contamination or a faulty reagent [21].
- Interpretation: Compare the volume of juice required to decolorize DCPIP to the volume of the standard Vitamin C solution required to do the same. The negative control validates that the color change is specific to the presence of Vitamin C-like substances.
Systematic Troubleshooting Pathway
The following diagram outlines a generalizable thought process for diagnosing experimental failures, integrating the use of controls and systematic checks.
Strategic Frameworks: DoE and Variance Component Analysis in Practice
Frequently Asked Questions (FAQs) & Troubleshooting
This section addresses common questions and issues researchers encounter when transitioning from One-Factor-At-a-Time (OFAT) approaches to Design of Experiments (DoE).
Q1: Why should we use DoE instead of the more intuitive OFAT method?
OFAT might seem straightforward, but it has major limitations. It involves changing a single factor while holding all others constant, which fails to capture interactions between factors and can lead to missing the true optimal conditions for your process [26] [24]. In contrast, DoE is a systematic, efficient framework that varies multiple factors simultaneously. This allows you to not only determine individual factor effects but also discover how factors interact, leading to more reliable and complete conclusions with fewer experimental runs [27].
Q2: What are the essential concepts we need to understand to start with DoE?
The key terminology in DoE includes [27]:
- Factor: An input parameter or variable that can be controlled (e.g., temperature, pH, concentration).
- Level: The specific value or setting of a factor during the experiment (e.g., temperature at 100°C and 200°C).
- Response: The output or measured result you are interested in (e.g., yield, purity, strength).
- Effect: The change in the response caused by varying a factor's level.
- Interaction: When the effect of one factor depends on the level of another factor.
Q3: Our experiments are often unstable, and the results drift over time. How can DoE help with this?
DoE incorporates fundamental principles to combat such variability and ensure robust results [26]:
- Randomization: Performing experimental runs in a random order helps eliminate the influence of uncontrolled variables and "noise," such as instrument drift or environmental changes.
- Replication: Repeating entire experimental runs allows you to estimate the inherent variability in your process, providing a more reliable measure of factor effects.
- Blocking: When full randomization is impossible (e.g., across different batches of raw material), blocking lets you group similar experimental units to account for this known source of variation.
Q4: We tried a simple 2-factor DoE, but the results were confusing. How do we quantify the effect of each factor?
The effect of a factor is calculated as the average change in the response when the factor moves from its low level to its high level. In a 2-factor design, you can compute this easily [26]. The table below shows data from a glue bond strength experiment.
| Experiment | Temperature | Pressure | Strength (lbs) |
|---|---|---|---|
| #1 | 100°C | 50 psi | 21 |
| #2 | 100°C | 100 psi | 42 |
| #3 | 200°C | 50 psi | 51 |
| #4 | 200°C | 100 psi | 57 |
- Effect of Temperature: (Strength at High Temp - Strength at Low Temp) =
(51 + 57)/2 - (21 + 42)/2 = 22.5 lbs - Effect of Pressure: (Strength at High Pressure - Strength at Low Pressure) =
(42 + 57)/2 - (21 + 51)/2 = 13.5 lbs[26]
This quantitative analysis clearly shows that temperature has a stronger influence on bond strength under these experimental conditions.
OFAT vs. DoE: A Quantitative Comparison
The following table summarizes the core differences between the OFAT and DoE approaches, highlighting why DoE is superior for understanding complex systems [27].
| Aspect | One-Factor-At-a-Time (OFAT) | Design of Experiments (DoE) |
|---|---|---|
| Efficiency | Inefficient; can require many runs to explore a multi-factor space. | Highly efficient; studies multiple factors simultaneously with fewer runs. |
| Interactions | Cannot detect interactions between factors. | Systematically identifies and quantifies interactions. |
| Optimal Conditions | High risk of finding only sub-optimal conditions. | Reliably identifies true optimal conditions and regions. |
| Statistical Robustness | Does not easily provide measures of uncertainty or significance. | Provides a model with statistical significance for effects. |
| Region of Operation | Cannot establish a region of acceptable results, making it hard to set robust operating tolerances. | Can map a response surface to define a robust operating window. |
Experimental Protocol: Conducting a Basic Two-Level Factorial Design
This protocol provides a step-by-step methodology for setting up and analyzing a simple yet powerful 2-factor DoE, a foundational design for source of variation analysis.
Pre-Experimental Planning
- Define Objective: Clearly state the goal (e.g., "Maximize the yield of Active Pharmaceutical Ingredient (API) synthesis").
- Identify Inputs & Outputs: Create a process map. Consult with subject matter experts to select the factors (inputs) to investigate and decide on the response (output) to measure [26]. Use a variable measure (e.g., yield percentage) rather than an attribute (pass/fail) [26].
- Select Factor Levels: For each factor, choose realistic "high" and "low" levels you wish to investigate (e.g., Reaction Temperature: 150°C and 200°C; Catalyst Concentration: 1.0 mol% and 2.0 mol%) [26].
Design Matrix Construction
A full factorial design for k factors requires 2^k runs. For a 2-factor experiment, this means 4 runs. The design matrix can be created using coded values (-1 for low level, +1 for high level) to standardize factors and simplify analysis [26] [27].
| Standard Order | Run Order (Randomized) | Factor A (Temp.) | Factor B (Catalyst) | Response (API Yield %) |
|---|---|---|---|---|
| 1 | 3 | -1 (150°C) | -1 (1.0 mol%) | To be measured |
| 2 | 1 | -1 (150°C) | +1 (2.0 mol%) | To be measured |
| 3 | 4 | +1 (200°C) | -1 (1.0 mol%) | To be measured |
| 4 | 2 | +1 (200°C) | +1 (2.0 mol%) | To be measured |
Note: Run order should be randomized to avoid confounding with lurking variables [26].
Execution & Data Collection
- Execute the experiments according to the randomized run order.
- Carefully measure and record the response for each run.
Data Analysis and Model Interpretation
- Calculate Main Effects: Use the method shown in FAQ #4 to quantify the effect of each factor.
- Calculate Interaction Effects: Expand the design matrix to include an interaction column (the mathematical product of the coded levels of Factor A and B). Calculate the interaction effect similarly to the main effects [26].
- Build a Predictive Model: The data can be used to fit a linear model:
Predicted Yield = β₀ + β₁*(Temp) + β₂*(Catalyst) + β₁₂*(Temp*Catalyst). The coefficients (β) are estimated from the data, creating a statistical model that can predict the response across the experimental region [24].
The Scientist's Toolkit: Essential Reagents & Materials for a DoE Workflow
While the specific materials depend on the experiment, the following table outlines key conceptual "reagents" and tools essential for a successful DoE.
| Item | Function in DoE Context |
|---|---|
| Coded Factor Levels | Standardizes factors with different units (e.g., °C, mol%, psi) to a common scale (-1, +1), simplifying analysis and comparison of effect magnitudes [27]. |
| Random Number Generator | A tool (software or simple method) to randomize the run order, a critical step for validating the statistical conclusions of the experiment [26]. |
| Design Matrix | The master plan of the experiment. It specifies the exact settings for each factor for every experimental run, ensuring a systematic and efficient data collection process [26] [27]. |
| Statistical Software | Essential for analyzing data from more complex designs, performing significance testing, building predictive models, and creating visualizations like response surface plots [24] [27]. |
DoE Workflow and Interaction Logic
The following diagram illustrates the logical workflow for implementing a DoE strategy, from planning to optimization, and how it effectively uncovers interactions between factors that OFAT misses.
This technical support guide provides researchers, scientists, and drug development professionals with practical troubleshooting guidance for implementing screening designs in experimental research. Screening designs are specialized experimental plans used to identify the few significant factors affecting a process or outcome from a long list of many potential variables [28] [29]. This resource addresses common implementation challenges and provides methodological support for effectively applying these techniques in source of variation analysis.
Understanding Screening Designs
What are Screening Designs and When Should They Be Used?
Screening designs, often called fractional factorial designs, are experimental strategies that systematically identify the most influential factors from many potential variables using a relatively small number of experimental runs [30] [29]. They operate on the "sparsity of effects" principle, which states that typically only a small fraction of potential factors will have significant effects on the response variable [29].
You should consider using screening designs when:
- You have many potential factors to study (typically 5 or more)
- The important factors are unknown among many candidates
- You need to conserve resources by reducing experimental runs
- You are in the early stages of process understanding [30] [28] [29]
These designs are particularly valuable in drug development and manufacturing processes where initial factor spaces can be large, and resource constraints make full factorial experimentation impractical.
How Screening Designs Compare to Other Experimental Approaches
Screening designs differ significantly from full factorial designs in both purpose and execution. The table below summarizes these key differences:
Table: Comparison of Screening Designs and Full Factorial Designs
| Characteristic | Screening Designs | Full Factorial Designs |
|---|---|---|
| Primary Purpose | Identify significant main effects | Characterize all effects and interactions |
| Number of Runs | Efficient, reduced runs | Comprehensive, all combinations |
| Information Obtained | Main effects (some interactions) | All main effects and interactions |
| Resource Requirements | Lower cost and time | Higher cost and time |
| Experimental Stage | Early investigation | Detailed characterization |
| Resolution | Typically III or IV [28] | V or higher |
Experimental Protocols and Methodologies
Screening Design Workflow
The following diagram illustrates the standard workflow for conducting a screening design experiment:
Types of Screening Designs
Several specialized screening designs are available, each with distinct characteristics and applications. The table below compares the most common approaches:
Table: Comparison of Screening Design Types
| Design Type | Key Characteristics | Optimal Use Cases | Limitations |
|---|---|---|---|
| 2-Level Fractional Factorial | Estimates main effects while confounding interactions; Resolution III-IV [28] | Initial screening with many factors; Limited runs available | Interactions confounded with main effects |
| Plackett-Burman | Very efficient for many factors; Resolution III [28] | Large factor screens (>10 factors); Minimal runs possible | Assumes interactions negligible |
| Definitive Screening | Estimates main effects, quadratic effects, and two-way interactions | When curvature or interactions suspected; Follow-up studies | Requires more runs than traditional methods [30] |
Essential Research Reagent Solutions
The following reagents and materials are fundamental for implementing screening designs in pharmaceutical and biotechnology research:
Table: Essential Research Reagents for Experimental Implementation
| Reagent/Material | Function/Purpose | Application Context |
|---|---|---|
| Process Factors | Variables manipulated during experimentation | Blend time, pressure, pH, temperature, catalyst concentration [29] |
| Response Measurement Tools | Quantify experimental outcomes | Yield determination, impurity analysis, potency assays [29] |
| Center Points | Replicate runs at middle factor levels | Detect curvature, estimate pure error [29] |
| Blocking Factors | Account for systematic variability | Batch differences, operator changes, day effects |
Troubleshooting Guide
Common Experimental Issues and Solutions
Table: Screening Design Troubleshooting Guide
| Problem/Error | Potential Causes | Solutions |
|---|---|---|
| Inability to Detect Significant Effects | Insufficient power; Too much noise; Factor ranges too narrow | Increase replication; Control noise factors; Widen factor ranges |
| Confounded Effects | Low resolution design; Aliased main effects and interactions | Use higher resolution design; Apply foldover technique to de-alias [30] |
| Curvature Detected in Response | Linear model inadequate; Quadratic effects present | Add axial points for RSM; Use definitive screening design [30] [29] |
| High Experimental Variation | Uncontrolled noise factors; Measurement system variability | Identify and control noise factors; Improve measurement precision |
Resolving Confounding in Screening Designs
The following diagram illustrates the relationship between design resolution and effect confounding, along with potential resolution strategies:
Frequently Asked Questions (FAQs)
Design Selection and Implementation
What is the minimum number of runs required for a screening design? The minimum run requirement depends on the number of factors and the design type. For a fractional factorial design with k factors, the minimum is typically 2^(k-p) runs, where p determines the fraction. Plackett-Burman designs can screen n-1 factors in n runs, where n is a multiple of 4 [30] [28].
When should I use a Plackett-Burman design versus a fractional factorial design? Use Plackett-Burman designs when you have a very large number of factors (12+) and can assume interactions are negligible. Fractional factorial designs are preferable when you suspect some interactions might be important and you need the ability to estimate them after accounting for main effects [30].
How do I handle categorical factors in screening designs? Most screening designs can accommodate categorical factors by assigning level settings appropriately. For example, a 2-level categorical factor (such as Vendor A/B or Catalyst Type X/Y) can be directly incorporated into the design matrix. For categorical factors with more than 2 levels, specialized design constructions may be necessary [29].
Analysis and Interpretation
How do I interpret the resolution of a screening design? Resolution indicates the degree of confounding in the design. Resolution III designs confound main effects with two-factor interactions. Resolution IV designs confound main effects with three-factor interactions but not with two-factor interactions. Resolution V designs confound two-factor interactions with other two-factor interactions but not with main effects [30] [28].
What should I do if I detect significant curvature in my screening experiment? If center points indicate significant curvature, consider adding axial points to create a response surface design, transitioning to a definitive screening design that can estimate quadratic effects, or narrowing the experimental region to a more linear space [29].
How many center points should I include in my screening design? Typically, 3-5 center points are sufficient for most screening designs. This provides enough degrees of freedom to estimate pure error and test for curvature without excessively increasing the total number of runs [29].
Advanced Applications
Can screening designs be used for mixture components in formulation development? Yes, specialized screening designs exist for mixture components where the factors are proportions of ingredients that must sum to 1. These designs often use simplex designs or special fractional arrangements to efficiently screen many components.
How do I handle multiple responses in screening designs? Analyze each response separately initially, then create overlay plots or desirability functions to identify factor settings that simultaneously satisfy multiple response targets. This is particularly valuable in pharmaceutical development where multiple quality attributes must be optimized [29].
What sequential strategies are available if my initial screening design provides unclear results? If results are ambiguous, consider foldover designs to de-alias effects, adding axial points to check for curvature, or conducting a follow-up fractional factorial focusing only on the potentially significant factors identified in the initial screen [30].
Factorial Designs for Analyzing Factor Interactions
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of factorial design over testing one factor at a time (OFAT)?
Factorial designs allow you to study the interaction effects between multiple factors simultaneously, which OFAT approaches completely miss [31]. When factors interact, the effect of one factor depends on the level of another. For instance, a specific drug dosage (Factor A) might only be effective when combined with a particular administration frequency (Factor B). A OFAT experiment could lead you to conclude the dosage is ineffective, while a factorial design would reveal this critical interaction [31] [32]. Furthermore, factorial designs are more efficient, providing more information—on multiple factors and their interactions—with fewer resources and experimental runs than conducting multiple separate OFAT experiments [31] [33].
Q2: How do I interpret a significant interaction effect?
A significant interaction effect indicates that the effect of one independent variable on the response is different at different levels of another independent variable [33]. You should not interpret the main effects (the individual effect of each factor) in isolation, as they can be misleading [31].
The best way to interpret an interaction is graphically, using an interaction plot:
- Non-parallel lines suggest an interaction is present [34] [35].
- Crossing lines indicate a strong interaction, where the effect of one factor completely reverses depending on the level of the other factor [35].
For example, in a plant growth study, the effect of a fertilizer (Factor A) might be positive at high sunlight (Factor B) but negative at low sunlight. The interaction plot would show non-parallel lines, and the analysis would reveal a significant interaction term [35].
Q3: My experiment has many potential factors. How can I manage the number of experimental runs?
With a full factorial design, the number of runs grows exponentially with each additional factor (2^k for a 2-level design with k factors) [36]. To manage this, researchers use screening designs:
- Fractional Factorial Designs: These use a carefully chosen subset (a fraction) of the full factorial runs. This allows you to efficiently screen many factors to identify the few that are most important, though some higher-order interactions may be confounded with main effects [37] [38].
- Definitive Screening Designs (DSDs): These are advanced, highly efficient designs that allow for screening a large number of factors with a minimal number of runs and can detect curvature in the response [38].
The key is to use these screening designs early in your experimentation process to narrow down the field of factors before conducting a more detailed full or larger fractional factorial study on the critical few [37].
Troubleshooting Guides
Problem 1: The experimental error is too high, obscuring factor effects.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Excessive variability in raw materials or process equipment. | Review records of raw material batches and equipment calibration. Check control charts for the process if available. | Implement stricter material qualification. Use blocking in your experimental design to account for known sources of variation like different batches or machine operators [37] [36]. |
| Uncontrolled environmental conditions. | Monitor environmental factors (e.g., temperature, humidity) during experiments to see if they correlate with high-variability runs. | Control environmental factors if possible. Otherwise, use blocking to group experiments done under similar conditions [36]. |
| Measurement system variability. | Conduct a Gage Repeatability and Reproducibility (Gage R&R) study. | Improve measurement procedures. Calibrate equipment more frequently. Increase the number of replications for each experimental run to get a better estimate of pure error [36]. |
Problem 2: The analysis shows no significant main effects or interactions.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Factor levels were set too close together. | Compare the range of your factor levels to the typical operating range or known process variability. The effect of the change might be smaller than the background noise. | Increase the distance between the high and low levels of your factors to evoke a stronger, more detectable response, provided it remains within a safe and realistic range [38]. |
| Insufficient power to detect effects. | Check the number of experimental runs and replications. A very small experiment has a high risk of Type II error (missing a real effect). | Increase the sample size or number of replications. Use power analysis before running the experiment to determine the necessary sample size [32]. |
| Important factors are missing from the design. | Perform a cause-and-effect analysis (e.g., Fishbone diagram, FMEA) to identify other potential influencing variables. | Conduct further screening experiments with a broader set of potential factors based on process knowledge and brainstorming [38]. |
Problem 3: The regression model has poor predictive ability.
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| The relationship between a factor and the response is curved (non-linear). | Check residual plots from your analysis for a clear pattern (e.g., a U-shape). A 2-level design can only model linear effects. | Move from a 2-level factorial to a 3-level design or a Response Surface Methodology (RSM) design like a Central Composite Design, which can model curvature (quadratic effects) [36]. |
| The model is missing important interaction terms. | Ensure your statistical model includes all potential interaction terms and that the ANOVA or regression analysis tests for their significance. | Re-analyze the data, explicitly including interaction terms in the model. A factorial design is orthogonally capable of estimating these interactions [31] [37]. |
Key Experimental Protocols
Protocol 1: Setting Up a Basic 2x2 Factorial Experiment
This protocol outlines the steps for designing a simple two-factor, two-level factorial experiment [31] [35].
- Define the Objective: Clearly state the research question and the response variable you are measuring.
- Select Factors and Levels: Choose two factors (e.g., Temperature, Concentration). For each, define a "low" and "high" level (e.g., 50°C and 70°C; 1% and 2%). These levels should be sufficiently different to expect a measurable change in the response.
- Create the Experimental Matrix: This lists all possible combinations of the factor levels. For a 2x2 design, this results in 4 unique experimental conditions.
- Randomize the Run Order: Randomly assign the order in which you will perform the four experimental runs. This is critical to avoid confounding the factor effects with unknown lurking variables or time-based trends [31] [36].
- Execute Experiments and Collect Data: Carry out the experiments in the randomized order, carefully measuring the response variable for each run.
- Analyze the Data: Calculate the main effects and the interaction effect. This can be done using statistical software that performs ANOVA or regression analysis.
Table: Experimental Matrix for a 2x2 Factorial Design
| Standard Run Order | Randomized Run Order | Temperature | Concentration | Response (e.g., Yield) |
|---|---|---|---|---|
| 1 | 3 | Low (50°C) | Low (1%) | |
| 2 | 1 | High (70°C) | Low (1%) | |
| 3 | 4 | Low (50°C) | High (2%) | |
| 4 | 2 | High (70°C) | High (2%) |
Protocol 2: Calculating Main and Interaction Effects
This protocol provides the mathematical methodology for calculating effects from a 2x2 factorial experiment, which forms the basis for the statistical model [35].
The regression model for a 2-factor design with interaction is: y = β₀ + β₁x₁ + β₂x₂ + β₁₂x₁x₂ + ε [37] Where y is the response, β₀ is the intercept, β₁ and β₂ are the main effect coefficients, β₁₂ is the interaction coefficient, and ε is the random error.
The calculations for a 2x2 design can be done using the average responses at different factor levels:
- Main Effect of Factor A: (Average response at Ahigh) - (Average response at Alow)
- Main Effect of Factor B: (Average response at Bhigh) - (Average response at Blow)
- Interaction Effect AB: (Average response when A and B are at the same level) - (Average response when A and B are at different levels). More precisely, it is half the difference between the effect of A at high B and the effect of A at low B [35].
Table: Calculation of Effects from Experimental Data
| Factor A | Factor B | Response | Calculation Step | Value |
|---|---|---|---|---|
| Low | Low | 2 | Main Effect A = (9+5)/2 - (2+0)/2 | 6 |
| High | Low | 5 | Main Effect B = (2+9)/2 - (5+0)/2 | 3 |
| Low | High | 9 | Interaction AB = ( (9-2) - (5-0) ) / 2 | 1 |
| High | High | 9 |
Experimental Workflows and Relationships
Factorial Experiment Workflow
Visualizing Interaction Effects
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Reagents and Materials for Factorial Experiments
| Item | Function in Experiment | Example Application |
|---|---|---|
| Statistical Software (R, Minitab, etc.) | Used to randomize run order, create the experimental design matrix, and perform the statistical analysis (ANOVA, regression). | The FrF2 package in R can generate and analyze fractional factorial designs [37]. |
| Coding System (-1, +1) | A method for labeling the low and high levels of factors. Simplifies the design setup, calculation of effects, and fitting of regression models [35]. | A temperature factor with levels 50°C and 70°C would be coded as -1 and +1, respectively. |
| Random Number Generator | A tool (often part of software) to ensure the run order of experimental trials is randomized. This is a critical principle of DOE to avoid bias [31] [36]. | Used to create the "Randomized Run Order" column in the experimental matrix. |
| Blocking Factor | A variable included in the design to account for a known, nuisance source of variation (e.g., different days, raw material batches). It is not of primary interest but helps reduce experimental error [37] [36]. | If experiments must be run on two different days, "Day" would be included as a blocking factor to prevent day-to-day variation from obscuring the effects of the primary factors. |
| ANOVA Table | The primary statistical output used to determine the significance of the main and interaction effects by partitioning the total variability in the data [36] [33]. | The p-values in the ANOVA table indicate whether the observed effects are statistically significant (typically p < 0.05). |
Step-by-Step Guide to Variance Component Analysis
Variance Component Analysis (VCA) is a statistical technique used in experimental design to quantify and partition the total variability in a dataset into components attributable to different random sources of variation [39]. This method is particularly valuable for researchers and scientists in drug development who need to understand which factors in their experiments contribute most to overall variability, enabling more precise measurements and better study designs.
Within the broader thesis on experimental design for source of variation research, VCA provides a mathematical framework for making inferences about population characteristics beyond the specific levels studied in an experiment. This approach helps distinguish between fixed effects (specific, selected conditions) and random effects (factors representing a larger population of possible conditions) [40].
Key Concepts and Terminology
Variance components are estimates of the part of total variability accounted for by each specified random source of variability [39]. In a nested experimental design, these components represent the hierarchical structure of data collection.
The mathematical foundation of VCA relies on linear mixed models where the total variance (σ²total) is partitioned into independent components. For a simple one-way random effects model, this can be represented as: σ²total = σ²between + σ²within, where σ²between represents variability between groups and σ²within represents variability within groups [41].
Distinction between fixed and random effects is crucial: fixed effects refer to specific, selected factors where levels are of direct interest, while random effects represent factors where levels are randomly sampled from a larger population, with the goal of making inferences about that population [40].
Experimental Protocols and Methodologies
Basic Protocol for One-Way Random Effects Model
For researchers conducting initial VCA, the following step-by-step protocol provides a robust methodology:
Experimental Design Phase: Identify all potential sources of variation in your study. Determine which factors are fixed versus random effects. Ensure appropriate sample sizes for each level of nesting.
Data Collection: Collect data according to the hierarchical structure of your design. For example, in an assay validation study, this might include multiple replicates within runs, multiple runs within days, and multiple days within operators.
Model Specification: Formulate the appropriate linear mixed model. For a one-way random effects model: Yij = μ + αi + εij, where αi ~ N(0, σ²α) represents the random effect and εij ~ N(0, σ²_ε) represents residual error.
Parameter Estimation: Use appropriate statistical methods to estimate variance components. The ANOVA method equates mean squares to their expected values: σ²α = (MSbetween - MSwithin)/n and σ²ε = MS_within.
Interpretation: Express components as percentages of total variance to understand their relative importance.
Advanced Protocol for Complex Designs
For more complex experimental designs common in pharmaceutical research:
Handling Unbalanced Designs: Most real-world designs are unbalanced. Use restricted maximum likelihood (REML) estimation rather than traditional ANOVA methods for more accurate estimates [40].
Addressing Non-Normal Data: For non-normal data (counts, proportions), consider generalized linear mixed models or specialized estimation methods for discrete data [40].
Accounting for Spatial/Temporal Correlation: Incorporate appropriate correlation structures when data exhibit spatial or temporal dependencies to avoid misleading variance component estimates [40].
Incorporating Sampling Weights: For complex survey designs with nonproportional sampling, use sampling weights to ensure representative variance component estimates [40].
VCA Methodology Workflow
Troubleshooting Common Problems
Negative Variance Estimates
Problem: Statistical software returns negative estimates for variance components, which is theoretically impossible since variances cannot be negative.
Causes:
- Insufficient sample size: Too few levels of the random factor or too few replicates [42]
- Outliers: Extreme values that distort variance patterns [42]
- True variance is zero: The random effect may not actually contribute to variability [42]
- Unbalanced designs: Highly unequal group sizes can lead to estimation problems [42]
- Incorrect model specification: The assumed covariance structure may not match the data [42]
Solutions:
- Increase sample size: Ensure sufficient levels of random factors and adequate replication
- Check for outliers: Examine data for influential points and consider robust estimation methods
- Use bounded estimation: Apply methods that constrain estimates to non-negative values [43]
- Try different estimation methods: Use REML instead of ANOVA methods, or Bayesian approaches with proper priors
- Simplify the model: Remove unnecessary random effects if evidence suggests they contribute little variability
Small Sample Size Issues
Problem: Unreliable variance component estimates due to limited data.
Solutions:
- Use Satterthwaite approximation: For confidence intervals with small samples [39]
- Apply Modified Large Sample (MLS) method: Provides better coverage with small samples [39]
- Consider Bayesian methods: Incorporate prior information to stabilize estimates
Handling Unbalanced Designs
Problem: Unequal group sizes or missing data leading to biased estimates.
Solutions:
- Use likelihood-based methods: REML provides better estimates for unbalanced data than traditional ANOVA [40]
- Implement appropriate weighting: Use sampling weights for surveys with nonproportional sampling [40]
- Consider multiple imputation: For missing data mechanisms that are missing at random
Frequently Asked Questions (FAQs)
What is the difference between variance components and the total variance? Variance components partition the total variance into pieces attributable to different random sources. The total variance is the sum of these components, and its square root provides the total standard deviation. Note that standard deviations of components cannot be directly added to obtain the total standard deviation [41].
How do I choose between fixed and random effects in my model? Fixed effects represent specific conditions of direct interest, while random effects represent a sample from a larger population about which you want to make inferences. For example, if studying three specific laboratories, lab is a fixed effect; if studying laboratories representative of all possible labs, lab is a random effect [40].
What should I do if my software gives negative variance components? First, check your data for outliers and consider whether your sample size is adequate. If the issue persists, use estimation methods that constrain variances to non-negative values, such as the restricted maximum likelihood principle [43]. In some cases, setting the negative estimate to zero may be appropriate if it's small and not statistically significant.
How many levels do I need for a random factor? While there's no universal rule, having at least 5-10 levels is generally recommended for reasonable estimation of variance components. With fewer levels, the estimate may be unstable, potentially leading to negative variance estimates [42].
What is the difference between ANOVA and REML for estimating variance components? ANOVA methods equate mean squares to their expected values and solve the equations. REML is a likelihood-based approach that is generally more efficient, especially for unbalanced designs and when estimating multiple variance components. REML also produces unbiased estimates that are not affected by the fixed effects in the model [43] [40].
How can I calculate confidence intervals for variance components? Several methods exist:
- Exact method: Based on the F-distribution for innermost nested components [39]
- Satterthwaite approximation: Uses modified degrees of freedom [39]
- Modified Large Sample (MLS): Works well across various conditions [39] The choice depends on your specific design and sample size considerations.
Research Reagent Solutions
Table: Essential Materials for Variance Component Analysis Studies
| Item | Function | Example Applications |
|---|---|---|
| Statistical Software (R, SAS, JMP) | Parameter estimation and inference | All variance component analyses [44] [41] |
| Laboratory Information Management System (LIMS) | Tracking hierarchical data structure | Managing nested experimental designs [40] |
| Balanced Experimental Design Templates | Ensuring equal replication at all levels | Avoiding estimation problems in simple designs [40] |
| Sample Size Calculation Tools | Determining adequate replication | Planning studies to achieve target precision [42] |
| Data Simulation Software | Evaluating model performance | Testing estimation methods with known parameters |
Data Presentation and Interpretation
Table: Sample Variance Components Output for Assay Validation Study
| Component | Variance Estimate | % of Total | Standard Deviation | Interpretation |
|---|---|---|---|---|
| Between-Batch | 0.0053 | 42.6% | 0.0729 | Primary source of variability |
| Within-Batch | 0.0071 | 57.4% | 0.0840 | Secondary source |
| Total | 0.0124 | 100% | 0.1113 | Overall variability |
When interpreting such results, researchers should note that between-batch variability accounts for 42.6% of total variance, suggesting that differences between manufacturing batches contribute substantially to overall variability. This information can guide quality improvement efforts toward better batch-to-batch consistency.
Advanced Applications and Extensions
Multivariate Responses: VCA can be extended to multivariate outcomes using methods described in ecological statistics literature [40]. This allows researchers to partition variance in multiple correlated responses simultaneously.
Nonlinear Models: For non-normal data such as counts or proportions, specialized approaches include generalized linear mixed models or variance partitioning methods developed for binary and binomial data [40].
Power Analysis: Variance component estimates from pilot studies can inform sample size calculations for future studies by providing realistic estimates of the variance structure expected in main effects and error terms.
Advanced VCA Applications
Variance Component Analysis provides a powerful framework for understanding the structure of variability in experimental data, particularly in pharmaceutical research and development. By properly implementing the protocols outlined in this guide, researchers can accurately partition variability, identify major sources of variation, and focus improvement efforts where they will have the greatest impact. Proper attention to troubleshooting and methodological nuances ensures reliable results that support robust decision-making in drug development and scientific research.
Scientist's Toolkit: Key Research Reagent Solutions
Table 1: Essential Excipients and Their Functions in Tablet Formulation
| Category | Example Excipients | Primary Function |
|---|---|---|
| Diluents | Microcrystalline Cellulose (e.g., Avicel PH 102), Lactose | Increase bulk of tablet to facilitate handling and administration [45] [46]. |
| Binders | Hydroxypropyl Cellulose (e.g., Klucel), Pregelatinized Starch (e.g., Starch 1500) | Impart cohesiveness to the powder, ensuring the tablet remains intact after compression [45] [46]. |
| Disintegrants | Sodium Starch Glycolate, Croscarmellose Sodium | Facilitate tablet breakup in the gastrointestinal fluid after administration [45]. |
| Lubricants | Magnesium Stearate | Reduce friction during tablet ejection from the compression die [45] [46]. |
| Glidants | Colloidal Silicon Dioxide (e.g., Aerosil 200) | Improve powder flowability during the manufacturing process [46]. |
Frequently Asked Questions (FAQs) on DoE Fundamentals
Q1: Why should we use DoE instead of the traditional One-Factor-at-a-Time (OFAT) approach?
DoE is superior to OFAT because it allows for the simultaneous, systematic, and efficient evaluation of all potential factors. The key advantage is its ability to detect and quantify interactions between factors—something OFAT completely misses [24] [45] [47]. For example, the effect of a change in compression force on tablet hardness might depend on the level of lubricant used. While OFAT would not detect this, a properly designed DoE can, leading to a more robust and better-understood process [24].
Q2: What are the typical stages of a DoE study in formulation development?
A systematic DoE implementation follows these key stages [45] [48]:
- Define the Problem and Objectives: Clearly state what you want to achieve (e.g., maximize dissolution, optimize yield).
- Identify Factors and Responses: Brainstorm and select the input variables (e.g., excipient levels, process parameters) and the output measurements (e.g., hardness, assay, dissolution).
- Choose the Experimental Design: Select an appropriate design (e.g., Fractional Factorial for screening, Response Surface Methodology for optimization) based on the number of factors and the study's goal.
- Execute the Experiment: Run the experiments in a randomized order to avoid bias.
- Analyze the Data: Use statistical methods like Analysis of Variance (ANOVA) to identify significant factors and build models.
- Interpret Results and Implement: Determine the optimal factor settings and confirm the findings with validation runs.
Q3: How can risk management be integrated into DoE studies?
Risk management tools like Failure Mode and Effects Analysis (FMEA) can be used before a DoE to prioritize factors for experimentation. In FMEA, potential failure modes (e.g., "low tablet hardness") are identified, and their causes (e.g., "low binder concentration," "high lubricant level") are scored for severity, occurrence, and detectability. The resulting Risk Priority Number (RPN) helps screen and select the high-risk factors to include in the DoE, ensuring resources are focused on the most critical variables [49] [46].
Troubleshooting Guides
Issue 1: Uncontrolled Variation and High Noise Obscuring Signal
Problem: The analysis of your DoE data shows that the error term (noise) is very high, making it difficult to determine which factors are statistically significant.
Solutions:
- Implement Rigorous Controls: Ensure all factors not being tested are kept constant. Use the same equipment, raw material lots, and environmental conditions throughout the study [48].
- Automate Data Collection: Where possible, use automated systems for data logging and measurement to minimize human error and inconsistency [48].
- Conduct Pilot Runs: Perform small-scale pilot runs before the full experiment to check the feasibility of the design, identify unforeseen sources of variation, and refine measurement techniques [48].
- Blocking: If a known source of variation exists (e.g., using two different raw material batches over the course of the experiment), use the statistical principle of "blocking" to account for it in the experimental design and remove its effect from the experimental error.
Issue 2: The Model Fits the Data Poorly or Fails to Predict Accurately
Problem: The statistical model derived from the DoE has a low R² value or performs poorly in predicting outcomes during validation runs.
Solutions:
- Check for Curvature: The initial model might assume only linear relationships, but the true response might be curved. Add center points to your screening design to detect curvature. If significant, move to a Response Surface Methodology (RSM) design like Central Composite or Box-Behnken to model these non-linear effects [24] [48].
- Verify Factor Ranges: The ranges selected for the factors might be too narrow to elicit a clear signal. Based on process knowledge, consider widening the factor ranges in a subsequent experiment.
- Include Missing Factors: A critical process parameter might have been omitted from the initial experimental design. Revisit the risk assessment (e.g., FMEA) and brainstorming sessions to identify any potential missing factors [46].
Issue 3: The Number of Experimental Runs is Impractically Large
Problem: A full factorial design for evaluating all factors of interest would require too many runs, making the study too costly or time-consuming.
Solutions:
- Use a Screening Design: Employ highly efficient designs like Fractional Factorial or Plackett-Burman designs. These designs use a fraction of the runs required for a full factorial to identify the few vital factors from the many less important ones [48] [46] [47].
- Apply Quality Risk Management: Use FMEA to prioritize variables before experimentation. By focusing only on high-risk factors, you can reduce the number of factors in the initial screening design, dramatically cutting down the number of required runs [46].
- Leverage Prior Knowledge: Use historical data, literature, and pre-formulation studies to fix some factors at a known optimal level, thereby reducing the number of variables to be experimentally investigated [46].
Detailed Experimental Protocol: A DoE for Tablet Formulation Optimization
This protocol outlines a response surface study to optimize a simple immediate-release tablet formulation, building on the principles from the provided sources [45].
Objective
To define the optimal levels of critical formulation factors to achieve target Critical Quality Attributes (CQAs) for an immediate-release tablet.
Experimental Workflow
The following diagram illustrates the sequential stages of a typical DoE-based formulation development process.
Methods and Procedures
Materials:
- Active Pharmaceutical Ingredient (API)
- Excipients: Diluent (e.g., Microcrystalline Cellulose), Binder (e.g., Hydroxypropyl Cellulose), Disintegrant (e.g., Sodium Starch Glycolate), Lubricant (e.g., Magnesium Stearate) [45] [46].
Formulation and Processing:
- Weighing and Blending: Accurately weigh all components according to the experimental design. Blend the API, diluent, binder, and disintegrant in a twin-shell blender for a fixed time (e.g., 10 minutes).
- Lubrication: Add the lubricant to the blend and mix for a further fixed time (e.g., 2 minutes).
- Compression: Compress the final blend on a tablet press equipped with force monitoring. Keep machine settings like feeder speed and turret speed constant across all runs.
Experimental Design: Table 2: Box-Behnken Response Surface Design for Three Factors
| Standard Run Order | Binder Concentration (%) | Disintegrant Concentration (%) | Lubricant Concentration (%) |
|---|---|---|---|
| 1 | 1.0 (-1) | 2.0 (-1) | 0.5 (0) |
| 2 | 2.0 (+1) | 2.0 (-1) | 0.5 (0) |
| 3 | 1.0 (-1) | 5.0 (+1) | 0.5 (0) |
| 4 | 2.0 (+1) | 5.0 (+1) | 0.5 (0) |
| 5 | 1.0 (-1) | 3.5 (0) | 0.25 (-1) |
| 6 | 2.0 (+1) | 3.5 (0) | 0.25 (-1) |
| 7 | 1.0 (-1) | 3.5 (0) | 0.75 (+1) |
| 8 | 2.0 (+1) | 3.5 (0) | 0.75 (+1) |
| 9 | 1.5 (0) | 2.0 (-1) | 0.25 (-1) |
| 10 | 1.5 (0) | 5.0 (+1) | 0.25 (-1) |
| 11 | 1.5 (0) | 2.0 (-1) | 0.75 (+1) |
| 12 | 1.5 (0) | 5.0 (+1) | 0.75 (+1) |
| 13 | 1.5 (0) | 3.5 (0) | 0.5 (0) |
| 14 | 1.5 (0) | 3.5 (0) | 0.5 (0) |
| 15 | 1.5 (0) | 3.5 (0) | 0.5 (0) |
Data Collection: For each experimental run, measure the following CQAs on a representative sample of tablets:
- Dissolution (% released at 30 min): Using USP apparatus.
- Tablet Hardness (kPa): Measured with a hardness tester.
- Friability (% loss): Measured using a friabilator.
Data Analysis and Interpretation
- Model Fitting: Input the data into statistical software (e.g., JMP, Design-Expert, Minitab). Perform multiple regression analysis to fit a quadratic model for each CQA [48].
- Analysis of Variance (ANOVA): For each model, check ANOVA to identify significant model terms (p-value < 0.05). Ensure the model is significant and there is a lack of fit is not significant.
- Optimization: Use the software's numerical and graphical optimization tools to find the factor settings that simultaneously meet the desired criteria for all CQAs (e.g., maximize dissolution, ensure hardness is within 10-15 kPa, and keep friability below 1.0%) [45].
- Validation: Conduct 2-3 confirmation batches at the predicted optimal settings to verify that the CQAs fall within the predicted ranges.
Solving Real-World Problems: Mitigating Bias and Enhancing Reproducibility
Troubleshooting Guides
Why do my experimental results sometimes show a cause-and-effect relationship that disappears upon deeper investigation?
This issue often arises from confounding variables, which are external factors that influence both the independent variable (the supposed cause) and the dependent variable (the supposed effect) in your study [50] [51]. A confounder can create a spurious association that does not reflect an actual causal relationship.
Troubleshooting Steps:
- Verify Confounder Criteria: Ensure the suspected variable meets all three conditions for a confounder [52]:
- It is a risk factor for or associated with the disease/outcome.
- It is associated with the primary exposure or independent variable.
- It is not a consequence of the exposure (not part of the causal pathway).
- Conduct Stratified Analysis: Separate your data into strata (subgroups) based on the levels of the potential confounder. If the association between your exposure and outcome differs significantly between the stratum-specific results and the overall (crude) result, confounding is likely present [53].
- Use Statistical Control: Employ multivariate regression models (e.g., linear or logistic regression) to include the potential confounder as a control variable. Compare the estimated effect of your independent variable before and after this adjustment. A substantial change indicates confounding [53] [50].
Diagram: The Structure of a Confounding Relationship
What is the most robust method to prevent confounding during the design phase of an experiment?
Randomization is widely considered the most effective method for controlling both known and unknown confounders at the study design stage [51].
Experimental Protocol: Randomization
- Objective: To randomly assign study subjects to exposure categories (e.g., treatment vs. control groups) to break any links between the exposure and confounders. This process creates groups that are comparable with respect to all potential confounding variables [53] [52].
- Procedure:
- Define your study population and obtain informed consent.
- For each eligible participant, generate a random assignment (e.g., via computer-generated random numbers) to one of the study groups.
- Ensure the allocation sequence is concealed until the moment of assignment to prevent selection bias.
- Proceed with the administration of the intervention or exposure according to the assigned groups.
- Key Consideration: Randomization is most effective with a sufficiently large sample size, as it ensures that all potential confounders have the same average value across different groups [51].
How can I control for confounding when my data has already been collected?
When experimental designs like randomization are not feasible, statistical methods after data collection are essential [53].
Method Selection Workflow
Experimental Protocol: Statistical Control via Regression
- Objective: To isolate the relationship between the independent and dependent variables by statistically holding constant the effects of one or more confounding variables [53] [50].
- Procedure:
- Model Selection: Choose an appropriate regression model based on your outcome variable type. Use linear regression for continuous outcomes or logistic regression for binary outcomes [53].
- Model Specification: Include your independent variable and all suspected confounding variables as predictors in the model. For example:
Outcome = Independent_Variable + Confounder1 + Confounder2 + ... + ConfounderN[50]. - Interpretation: The coefficient for your independent variable in this multiple regression model represents its effect on the outcome, adjusted for the confounders. This yields an adjusted odds ratio or risk ratio [53].
Frequently Asked Questions (FAQs)
What is the definitive difference between a confounding variable and an extraneous variable?
All confounding variables are extraneous variables, but not all extraneous variables are confounders [51]. The critical distinction lies in the causal structure:
- An extraneous variable is any variable that is not the primary focus of investigation but can potentially affect the dependent variable.
- A confounding variable is a specific type of extraneous variable that is related to both the independent variable and the dependent variable, thereby distorting their true relationship [51].
Can you provide a classic example of confounding?
A classic example is the observed association between coffee drinking and lung cancer [53] [50]. Early studies might have suggested that coffee causes lung cancer. However, smoking is a powerful confounder in this relationship because:
- Smoking is associated with coffee drinking (smokers are more likely to drink coffee).
- Smoking is a known cause of lung cancer.
- Smoking is not an effect of coffee drinking.
When smoking is accounted for, the apparent link between coffee consumption and lung cancer disappears [53].
I have limited sample size; what is the most efficient way to control for confounding?
When sample size is a constraint, restriction is a straightforward and efficient method [53] [51]. Instead of measuring and adjusting for a confounder, you simply restrict your study to only include subjects with the same value of that confounder. For example, if age is a potential confounder, you restrict your study to only include subjects aged 50-60 years. Since the confounder does not vary within your study sample, it cannot confound the relationship [51].
How do I know if I have successfully controlled for confounding?
You can assess the success of your control strategy by comparing the results of your analysis before and after adjusting for the confounder [53]:
- In stratification, compare the crude (unadjusted) estimate to the Mantel-Haenszel summary estimate. A significant difference indicates confounding was present and addressed.
- In regression, compare the coefficient of your independent variable in a simple model (without confounders) to its coefficient in a multiple model (with confounders). A meaningful change suggests successful control.
Comparison of Confounding Control Methods
| Method | Key Principle | Best Use Case | Major Advantage | Major Limitation |
|---|---|---|---|---|
| Randomization [53] [51] | Random assignment balances known and unknown confounders across groups. | Controlled experiments and clinical trials. | Controls for all potential confounders, even unmeasured ones. | Often impractical or unethical in observational studies. |
| Restriction [53] [51] | Limits study subjects to those with identical levels of the confounder. | When a few key confounders are known and sample size is sufficient. | Simple to implement and analyze. | Restricts sample size and generalizability; cannot control for other factors. |
| Matching [53] [51] | Pairs each subject in one group with a subject in another group who has similar confounder values. | Case-control studies where a comparison group is selected. | Improves efficiency and comparability in group comparisons. | Difficult to find matches for multiple confounders; can be labor-intensive. |
| Stratification [53] | Divides data into subgroups (strata) where the confounder is constant. | Controlling for one or two confounders with a limited number of strata. | Intuitively shows how the relationship changes across strata. | Becomes impractical with many confounders (leads to sparse strata). |
| Multivariate Regression [53] [50] | Statistically holds confounders constant to isolate the exposure-outcome effect. | Controlling for multiple confounders simultaneously, including continuous variables. | Highly flexible; can adjust for many variables at once. | Relies on correct model specification; can only control for measured variables. |
The Scientist's Toolkit: Key Reagents & Materials
This table details essential methodological "reagents" for diagnosing and controlling confounding in research.
| Item | Function in Experimental Design |
|---|---|
| Directed Acyclic Graphs (DAGs) | A visual tool used to map out presumed causal relationships between variables based on subject-matter knowledge. DAGs help formally identify which variables are confounders requiring control and which are not (e.g., mediators on the causal pathway) [54]. |
| Stratification Analysis | A diagnostic and control "reagent" that splits the dataset into homogeneous layers (strata) based on the value of a potential confounder. This allows the researcher to see if the exposure-outcome relationship is consistent across all strata [53]. |
| Mantel-Haenszel Estimator | A statistical formula applied after stratification. It produces a single summary effect estimate (e.g., an odds ratio) that is adjusted for the stratifying factor, providing a straightforward way to control for a confounding variable [53]. |
| Regression Models | Versatile statistical tools that function as multi-purpose controls. By including confounders as covariates in models like linear or logistic regression, researchers can statistically isolate the relationship between their primary variables of interest [53] [50]. |
| Pilot Studies / Literature Review | A foundational "reagent" for identifying potential confounders before a main study is launched. Domain knowledge and preliminary research are critical for building a comprehensive list of variables to measure and control [50]. |
Implementing Effective Randomization and Blinding
Troubleshooting Guides and FAQs
Troubleshooting Common Randomization Issues
Issue: My treatment groups ended up with unequal sizes and different baseline characteristics, especially in my small pilot study.
- Cause: This is a common risk when using simple randomization in studies with a small sample size. While random in nature, this method does not guarantee balance in group sizes or participant characteristics for small trials [55] [56].
- Solution: Implement restricted (block) randomization. This method ensures that after every few participants (a "block"), an equal number are assigned to each group. For example, in a two-group trial with a block size of 4, each block will contain 2 participants for Group A and 2 for Group B, maintaining perfect balance over time [55] [56]. Ensure the block size is not too small and is concealed from investigators to prevent prediction of the next assignment [55].
Issue: An investigator accidentally revealed the next treatment assignment because the randomization sequence was predictable.
- Cause: The method used for allocation concealment was inadequate. If the sequence is predictable (e.g., using alternation or open lists), investigators can consciously or unconsciously influence which participants are assigned to which group, introducing selection bias [55] [56].
- Solution:
- Use a centralized interactive response technology (IRT) system, such as an Interactive Web Response System (IWRS), to assign treatments in real-time after a participant is enrolled [55] [57].
- If an automated system is not feasible, use sequentially numbered, opaque, sealed envelopes prepared by an independent party. Eligibility must be confirmed before the envelope is opened [55].
Issue: I am running a multi-centre trial and need to ensure treatment groups are balanced for a key prognostic factor like disease severity.
- Cause: Simple or block randomization alone may not control for known, influential confounding variables across multiple sites [55] [58].
- Solution: Employ stratified randomization. First, participants are grouped into "strata" based on the prognostic factor (e.g., mild vs. severe disease). Then, within each stratum, a separate randomization procedure (like block randomization) is used to assign participants to treatment groups. This ensures a balanced distribution of that factor across all groups [55] [56] [58].
Table 1: Comparison of Common Randomization Methods
| Method | Key Principle | Best For | Advantages | Limitations |
|---|---|---|---|---|
| Simple Randomization [56] | Assigns each participant via a random process, like a coin toss or computer generator. | Large trials (typically > 200 participants) [56]. | Simple to implement; no predictability. | High risk of imbalanced group sizes and covariates in small samples. |
| Block Randomization [55] [56] | Participants are randomized in small blocks (e.g., 4, 6) to ensure equal group sizes at the end of each block. | Small trials or any study where maintaining equal group size over time is critical. | Guarantees balance in group numbers throughout the enrollment period. | If block size is known, the final assignment(s) in a block can be predicted. |
| Stratified Randomization [55] [56] | Randomization is performed separately within subgroups (strata) of participants who share a key prognostic factor. | Ensuring balance for specific, known confounding variables (e.g., age, study site, disease severity). | Controls for both known and unknown confounders within strata; increases study power. | Complexity increases with more stratification factors. |
Troubleshooting Common Blinding Issues
Issue: My intervention is a complex behavioral therapy. It's impossible to blind the therapists and participants. How do I prevent bias?
- Cause: The inherent nature of many complex interventions (e.g., surgery, physical therapy, educational programs) makes full blinding of participants and providers unfeasible [59].
- Solution: Implement a single-blind design with a focus on blinding the outcome assessors and the data analysts. Even if participants and caregivers know the treatment, having independent assessors who are unaware of group allocation collect and evaluate the endpoint data can significantly reduce detection bias [59] [56]. For patient-reported outcomes (PROMs), which are inherently unblinded, consider supplementing them with blinded objective measures or blinded adjudication of events [59].
Issue: My experimental drug and placebo look and taste different, risking unblinding.
- Cause: Inadequate matching of the sensory characteristics (sight, smell, taste, texture) of the investigational product and its control [60].
- Solution: Work with formulation experts to create a placebo that is identical in all physical attributes. Techniques include over-encapsulation for tablets and capsules or using opaque sleeves for syringes to mask the color and cloudiness of injectable liquids [60]. A thorough sensory evaluation during the product development phase is crucial.
Issue: An administrative email accidentally revealed treatment codes, potentially unblinding site staff.
- Cause: Human error during routine administrative tasks, such as sharing documents that link treatment group codes to specific participants [60].
- Solution:
- Develop a blinding procedures checklist based on the protocol to standardize communication and document handling [60].
- Implement strict access controls in electronic systems (IRT, EDC). Before sending any study-related information, always confirm the recipient's blinding status [60] [57].
- Ensure all personnel are trained on emergency unblinding protocols, which allow for controlled, individual unblinding in case of a medical emergency without compromising the entire study's blind [58].
Table 2: Levels of Blinding and Their Purpose
| Who is Blinded? | Term | Primary Purpose | Common Challenges |
|---|---|---|---|
| Participant | Single-Blind | Reduces performance bias (e.g., placebo effect) and psychological influences on outcomes. | Difficult with interventions that have distinctive sensory profiles or side effects. |
| Participant and Investigator/Provider | Double-Blind | Prevents bias in administration of care, management, and evaluation of outcomes by the care team. | Not feasible for many complex, behavioral, or surgical interventions [59]. |
| Outcome Assessor | Single-Blind (Assessor) | Minimizes detection (ascertainment) bias, as the person judging the outcome is unaware of the treatment. | Requires independent, trained personnel not involved in the intervention. Highly feasible even when participant/provider blinding is not [59]. |
| Participant, Provider, Outcome Assessor, and Data Analyst | Triple-Blind | Provides maximum protection against bias, including during data analysis and interpretation. | Requires robust system safeguards to prevent accidental unblinding through data reports or audit logs [57]. |
Frequently Asked Questions (FAQs)
Q1: What is the difference between randomization and allocation concealment?
- Randomization is the overall process of generating an unpredictable sequence for assigning interventions. It is the "why" behind having comparable groups [56].
- Allocation Concealment is the "how" – the specific technique used to implement that sequence while shielding it from the investigators enrolling participants. It secures the randomization process and prevents selection bias by ensuring the investigator cannot know or influence the next assignment before a participant is formally entered into the trial [55] [56]. Proper randomization requires both a random sequence generation and concealed allocation.
Q2: When is it acceptable to NOT use randomization or blinding? While randomization and blinding are gold standards, there are contexts where they may not be fully applicable:
- Randomization: May be challenging or unethical in some public health or cluster-randomized trials. In such cases, alternative designs must be rigorously justified, and their limitations acknowledged [55].
- Blinding: Is often not feasible for complex interventions (e.g., surgery, physical therapy) [59]. The 2025 SPIRIT guidelines emphasize transparent reporting of blinding status for all trial groups (participants, care providers, outcome assessors, data analysts) [61]. When blinding is not possible, the protocol should explicitly state who is unblinded and describe other methods to minimize bias, such as using objective outcome measures and independent blinded adjudication committees [59] [61].
Q3: What software tools are recommended for managing randomization and blinding in complex trials? Modern clinical trials rely on specialized software to ensure precision and auditability. The following table summarizes key tools available in 2025:
Table 3: Overview of 2025 Randomization & Trial Supply Management (RTSM) Tools
| Tool Name | Key Strengths | Best Suited For |
|---|---|---|
| Medidata RTSM [57] | End-to-end integration with the Medidata Clinical Cloud; robust features for stratification and mid-study updates. | Large, complex global trials requiring seamless data flow. |
| Suvoda IRT [57] | Highly configurable; rapid deployment; strong support for temperature-sensitive supply chains. | Oncology and other time-critical, complex studies. |
| 4G Clinical Prancer [57] | Uses natural language for configuration; fast startup; designed for adaptive designs. | Rare disease, gene therapy, and adaptive platform trials. |
| Almac IXRS 3 [57] | Proven stability and reliability; strong audit controls; extensive multilingual support. | Multinational Phase III trials with intense regulatory scrutiny. |
Essential Research Reagent Solutions
Table 4: Key Materials for Implementing Randomization and Blinding
| Item / Solution | Function in Experimental Design |
|---|---|
| Interactive Response Technology (IRT/IWRS) [55] [57] | Automates random treatment assignment and drug supply management in real-time, ensuring allocation concealment and providing a full audit trail. |
| Matched Placebo [60] | A physically identical but inactive version of the investigational product, crucial for maintaining the blind of participants and investigators. |
| Over-Encapsulation [60] | A technique where tablets are placed inside an opaque capsule shell to mask the identity of the active drug versus a placebo or comparator. |
| Sequentially Numbered, Opaque, Sealed Envelopes [55] | A low-tech but effective method for allocation concealment when electronic systems are not available; must be managed rigorously to prevent tampering. |
| Dummy Randomization Schedule [58] | A mock schedule used during the planning phase to preview randomization outputs and finalize procedures without breaking the blind for the actual trial. |
Experimental Workflow and Protocol Diagrams
Troubleshooting Guides
Guide 1: Resolving Low Statistical Power in Experimental Results
Problem: Your experiment failed to find a statistically significant effect, even though you suspect one exists. This often indicates low statistical power.
Symptoms:
- P-values consistently above 0.05 despite observable differences between groups
- Wide confidence intervals that include potentially important effects
- Inconsistent results across multiple similar studies
Troubleshooting Steps:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Verify Effect Size Estimation | More realistic power calculation |
| 2 | Check Sample Size Constraints | Identification of feasibility issues |
| 3 | Review Measurement Precision | Reduced standard deviation |
| 4 | Consider Alpha Level Adjustment | Appropriate balance of Type I/II errors |
| 5 | Evaluate Research Design | Improved efficiency and power |
Detailed Procedures:
- Recalculate Effect Size: Use pilot data or literature to establish realistic effect size expectations. Overestimated effect sizes are a primary cause of underpowered studies [62].
- Assess Sample Limitations: Determine if logistical constraints led to insufficient sampling. Even with large effect sizes, inadequate samples yield low power [63].
- Improve Measurement: Reduce standard deviation through more precise instruments or standardized protocols [64].
- Balance Error Risks: For pilot studies, consider alpha = 0.10 instead of 0.05 to reduce Type II error risk [63].
- Optimize Design: Switch to within-subjects designs when possible, as they typically provide more power than between-subjects designs with the same sample size [62].
Guide 2: Addressing Inconsistent Results Across Multiple Experiments
Problem: Similar experiments yield conflicting significant and non-significant findings.
Symptoms:
- Fluctuating P-values across study replications
- Effect sizes that vary substantially between studies
- Inability to draw definitive conclusions from the body of evidence
Troubleshooting Steps:
| Step | Action | Key Considerations |
|---|---|---|
| 1 | Conduct Power Analysis | Use smallest effect size of interest |
| 2 | Standardize Protocols | Ensure consistent measurement |
| 3 | Check Sample Homogeneity | Assess population variability |
| 4 | Review Analytical Methods | Verify appropriate statistical tests |
| 5 | Perform Meta-analysis | Combine results quantitatively |
Detailed Procedures:
- Retrospective Power Analysis: Calculate the power of each completed study using the actual sample size and observed effect size. This helps interpret why some studies may have failed to detect effects [64].
- Methodology Alignment: Ensure consistent participant selection criteria, measurement tools, and experimental conditions across studies [65].
- Variability Assessment: Examine whether studies with null findings had more heterogeneous samples, increasing standard deviation and reducing power [64].
- Statistical Method Audit: Confirm that all studies used appropriate statistical tests and met necessary assumptions [63].
- Cumulative Analysis: Combine results using meta-analytic techniques to determine if the overall evidence supports an effect despite individual study inconsistencies [65].
Frequently Asked Questions (FAQs)
FAQ 1: What is statistical power and why is it crucial for my research?
Statistical power is the probability that your test will correctly reject a false null hypothesis—in other words, the chance of detecting a real effect when it exists [62]. Power is crucial because:
- Low-powered studies risk missing important effects (Type II errors) [63]
- Inadequate power makes findings questionable even when statistically significant
- Funding agencies often require power analysis in grant proposals [65]
- Ethically, underpowered clinical trials may expose participants to risk without scientific benefit [64]
FAQ 2: How do I determine the appropriate sample size for my experiment?
Sample size determination requires specifying several parameters [64]:
| Parameter | Definition | Impact on Sample Size |
|---|---|---|
| Effect Size | Magnitude of the difference or relationship you want to detect | Larger effect → Smaller sample needed |
| Alpha (α) | Probability of Type I error (false positive) | Lower alpha → Larger sample needed |
| Power (1-β) | Probability of detecting a true effect | Higher power → Larger sample needed |
| Variability | Standard deviation in your measurements | Higher variability → Larger sample needed |
Use the formula for comparing two means [63]:
Where σ = pooled standard deviation, δ = difference between means
FAQ 3: What is the difference between statistical significance and clinical relevance?
Statistical significance indicates that an observed effect is unlikely due to chance, while clinical relevance means the effect size is large enough to matter in practical applications [65]. A study may have:
- Statistical significance but not clinical relevance: With a large sample, even tiny, unimportant effects can be statistically significant
- Clinical relevance but not statistical significance: With a small sample, important effects may not reach statistical significance
Always interpret results in context of effect size and practical implications, not just p-values [63].
FAQ 4: Can I calculate power after conducting my study (post-hoc power)?
Technically yes, but post-hoc power analysis is generally discouraged, especially when you found statistically significant results [64]. For non-significant results, post-hoc power can indicate how likely you were to detect effects, but it's more informative to report confidence intervals around your effect size estimate [62].
FAQ 5: What are common mistakes in power analysis and how can I avoid them?
Common mistakes include [63] [65]:
| Mistake | Consequence | Solution |
|---|---|---|
| Overestimating effect size | Underpowered study | Use conservative estimates from literature |
| Ignoring multiple comparisons | Inflated Type I error | Adjust alpha (e.g., Bonferroni) |
| Neglecting practical constraints | Unrealistic sample size goals | Plan feasible recruitment strategies |
| Using default settings without justification | Inappropriate assumptions | Justify all parameters based on evidence |
Sample Size Calculation Tables
Table 1: Recommended Parameter Values for Sample Size Calculation
| Parameter | Standard Value | Pilot Study Value | High-Stakes Value |
|---|---|---|---|
| Alpha (α) | 0.05 | 0.10 | 0.01 or 0.001 |
| Power (1-β) | 0.80 | 0.70 | 0.90 or 0.95 |
| Effect Size | Varies by field | Based on preliminary data | Minimal important difference |
Table 2: Sample Size Requirements for Common Statistical Tests
| Test Type | Small Effect | Medium Effect | Large Effect |
|---|---|---|---|
| Independent t-test | 786 per group | 128 per group | 52 per group |
| Paired t-test | 394 pairs | 64 pairs | 26 pairs |
| Chi-square test | 785 per group | 87 per group | 39 per group |
| Correlation | 782 | 85 | 28 |
Note: Calculations assume α=0.05, power=0.80, two-tailed tests. Actual requirements may vary based on specific conditions [63].
Experimental Protocols
Protocol 1: A Priori Sample Size Determination
Purpose: To determine the required sample size before conducting an experiment.
Materials Needed:
- Literature on similar studies for effect size estimation
- Statistical software (e.g., G*Power, R, SAS)
- Knowledge of expected variability in measurements
Procedure:
- Define Primary Outcome: Identify the main variable you will analyze.
- Establish Effect Size: Based on:
- Minimal clinically important difference
- Previous research findings
- Practical significance thresholds
- Set Error Rates: Typically α=0.05, power=0.80 [63]
- Choose Statistical Test: Select appropriate analysis method
- Calculate Sample Size: Using software or manual formulas
- Account for Attrition: Increase sample by 10-20% if dropout is expected
Validation: Conduct sensitivity analysis with different effect size assumptions.
Protocol 2: Power Analysis for Grant Applications
Purpose: To justify requested resources through statistical power calculations.
Materials Needed:
- Preliminary data or published literature
- Sample size calculation software
- Study protocol details
Procedure:
- Justify Effect Size: Provide rationale for expected effect size using:
- Effect sizes from similar published studies
- Clinical or practical significance thresholds
- Pilot study results if available
- Specify Analysis Method: Detail primary statistical analysis approach
- Document Assumptions: Clearly state all parameters used in calculations
- Present Multiple Scenarios: Show sample needs for different effect sizes
- Address Feasibility: Demonstrate recruitment capability within timeline
Deliverable: Power analysis section for grant proposal with clear justification of sample size request [65].
Visual Workflows and Diagrams
Research Reagent Solutions
Table 3: Essential Tools for Power Analysis and Sample Size Determination
| Tool Name | Type | Primary Function | Key Features |
|---|---|---|---|
| G*Power | Software | Power analysis for various tests | Free, user-friendly, wide test coverage [62] |
| Sample Size Tables | Reference | Quick sample size estimates | Handy for preliminary planning [63] |
| Effect Size Calculators | Computational | Convert results to effect sizes | Enables comparison across studies [65] |
| Online Sample Size Calculators | Web-based tools | Immediate sample size estimates | Accessible, no installation required [64] [66] |
| Statistical Software Packages | Comprehensive | Advanced power analysis | SAS, R, SPSS with specialized power procedures [63] |
The PDCA (Plan-Do-Check-Act) Cycle for Continuous Process Improvement
The Plan-Do-Check-Act (PDCA) cycle is a systematic, iterative management method used for the continuous improvement of processes and products. Rooted in the scientific method, it provides a simple yet powerful framework for structuring experimentation, problem-solving, and implementing change [67] [68]. For researchers, scientists, and drug development professionals, the PDCA cycle offers a disciplined approach to experimental design, data analysis, and process optimization, which is fundamental for rigorous source of variation analysis.
The cycle consists of four core stages, as illustrated in the workflow below:
Originally developed by Walter Shewhart and later popularized by W. Edwards Deming, the PDCA cycle (also known as the Deming Cycle or Shewhart Cycle) has become a cornerstone of quality management and continuous improvement in various industries, including pharmaceutical development and scientific research [69] [70]. Its relevance to experimental design lies in its structured approach to testing hypotheses, controlling variation, and implementing evidence-based changes.
The Four Phases of PDCA: Detailed Experimental Protocols
Plan: Define the Experimental Framework
The Plan phase involves defining the problem, establishing objectives, and developing a detailed experimental protocol. For research professionals, this phase is critical for identifying potential sources of variation and designing experiments to investigate them [67] [71].
Key Activities:
- Problem Definition: Clearly articulate the specific process or quality issue to be addressed. Use data from previous experiments or process metrics to quantify the problem.
- Objective Setting: Establish SMART (Specific, Measurable, Achievable, Relevant, Time-bound) objectives for the improvement effort [71].
- Hypothesis Development: Formulate testable hypotheses about potential solutions and their expected impact on key output variables.
- Experimental Design: Plan data collection methods, determine sample sizes, identify control factors, and define measurement systems to ensure reliable results.
- Resource Allocation: Identify required personnel, equipment, and materials for executing the experiment.
Research Application Example: When investigating variation in assay results, the Plan phase would include identifying potential sources of variation (e.g., operator technique, reagent lot differences, environmental conditions), designing experiments to test each factor's contribution, and establishing protocols for controlled testing.
Do: Implement the Experiment
The Do phase involves executing the planned experiment on a small scale to test the proposed changes [67] [72]. This implementation should be controlled and carefully documented to ensure valid results.
Key Activities:
- Implementation: Execute the experimental protocol as designed, applying the proposed change or intervention.
- Data Collection: Systematically gather data according to the predefined measurement plan.
- Documentation: Record all experimental conditions, observations, and unexpected occurrences that might affect results.
- Control: Maintain strict adherence to the experimental protocol to minimize introducing additional variation.
Research Application Example: For a method transfer between laboratories, the Do phase would involve executing the comparative testing protocol across sites, with all laboratories following identical procedures and recording all data points and observations according to the pre-established plan.
Check: Analyze Results and Identify Learning
The Check phase involves evaluating the experimental results against the expected outcomes defined in the Plan phase [67] [71]. This is where statistical analysis of variation is particularly valuable.
Key Activities:
- Data Analysis: Perform statistical analysis to determine if observed differences are statistically significant and practically important.
- Comparison to Hypotheses: Evaluate whether the experimental results support the initial hypotheses.
- Variation Analysis: Examine both common cause and special cause variation in the results.
- Root Cause Investigation: If results deviate from expectations, investigate potential causes.
- Learning Documentation: Clearly document insights gained from the experiment.
Research Application Example: In analytical method validation, the Check phase would include statistical analysis of method precision, accuracy, and robustness data to determine if the method meets pre-defined acceptance criteria and identifies significant sources of variation.
Act: Standardize or Refine
The Act phase involves implementing the validated changes on a broader scale or refining the approach based on the experimental findings [67] [72].
Key Activities:
- Standardization: If the change was successful, update standard operating procedures (SOPs), work instructions, and training materials to incorporate the improvement.
- Broad Implementation: Roll out the validated change to all relevant processes, systems, or locations.
- Replanning: If the change was not successful, use the learning to refine the approach and begin a new PDCA cycle.
- Monitoring: Establish ongoing monitoring to ensure the improvement is sustained and to identify any new sources of variation.
Research Application Example: Following successful method optimization, the Act phase would involve updating the analytical procedure, training all relevant personnel on the improved method, and implementing ongoing system suitability testing to monitor method performance.
PDCA for Source of Variation Analysis
The PDCA cycle provides a structured approach for investigating, analyzing, and controlling sources of variation in research and development processes. The table below outlines common sources of variation in experimental systems and corresponding PDCA approaches for addressing them.
Table: Common Sources of Variation and PDCA-Based Mitigation Strategies
| Source of Variation | Impact on Experimental Systems | PDCA Phase for Addressing | Typical Mitigation Approach |
|---|---|---|---|
| Instrument Variation | Analytical measurement error, reduced method precision | Check | Regular calibration, preventive maintenance, system suitability testing |
| Operator Technique | Systematic bias, increased variability | Act/Plan | Standardized training, certification programs, procedure clarification |
| Reagent/Lot Differences | Shift in baseline results, calibration drift | Plan/Do | Vendor qualification, bridging studies, specification establishment |
| Environmental Conditions | Uncontrolled external factors affecting results | Plan/Check | Environmental monitoring, controlled conditions, stability studies |
| Sample Handling | Introduction of pre-analytical variables | Do/Act | Standardized collection protocols, stability validation, handling training |
| Temporal Effects | Drift over time, seasonal impacts | Check | Trend analysis, control charts, periodic review |
In complex experimental systems, multiple factors may interact to produce variation. A two-way ANOVA or factorial experimental design is often necessary to disentangle these effects and identify significant interactions [73]. The PDCA framework supports this structured investigation through iterative cycles of hypothesis testing and refinement.
Troubleshooting Guide: Common Experimental Issues
FAQ: Addressing Common PDCA Implementation Challenges
Q: What should I do if the Check phase reveals no significant improvement? A: This is a common outcome that provides valuable learning. Return to the Plan phase with the new knowledge gained. Consider whether the root cause was correctly identified, if the intervention was properly executed, or if additional factors need investigation. The iterative nature of PDCA means that "failed" cycles still generate insights for improvement [67] [72].
Q: How can we maintain momentum when multiple PDCA cycles are needed? A: Document and celebrate small wins and learning from each cycle, even if the ultimate goal hasn't been achieved. Establish a visual management system to track progress across multiple cycles. Ensure leadership support recognizes the value of the learning process, not just final outcomes [71].
Q: What's the best approach when we discover unexpected interaction effects between variables? A: Unexpected interactions are valuable findings. In the Check phase, document these interactions thoroughly. In the subsequent Act phase, initiate a new PDCA cycle specifically designed to investigate these interactions through designed experiments (e.g., factorial designs) to better understand the system behavior [73].
Q: How do we prevent backsliding after successful implementation? A: The Act phase should include robust standardization (updated SOPs, training), monitoring mechanisms (control charts, periodic audits), and clear accountability for maintaining the improved state. Consider subsequent PDCA cycles to further refine and optimize the process [67] [70].
Troubleshooting Experimental Discrepancies
When experimental results show unexpected variation or discrepancies, consider these common issues:
- Measurement System Problems: Verify calibration and precision of instruments. Conduct gage R&R studies to quantify measurement error.
- Uncontrolled Environmental Factors: Review monitoring data for temperature, humidity, or other relevant conditions that may have deviated from specifications.
- Protocol Adherence Issues: Audit whether all operators followed the exact same procedures and timing.
- Sample Integrity Concerns: Investigate potential issues with sample collection, handling, or storage that could introduce variation.
- Data Integrity Problems: Review data transcription, calculation methods, and statistical analysis for errors [74].
For complex variation issues, consider expanding the experimental design to include more factors or levels to better capture the system's behavior and interaction effects [73].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents and Materials for Experimental Process Improvement
| Reagent/Material | Function in Experimental Process | Quality Considerations | Variation Control Applications |
|---|---|---|---|
| Reference Standards | Calibration and method validation | Purity, stability, traceability | Establishing measurement baselines, quantifying systematic error |
| Certified Reference Materials | Quality control, method verification | Documented uncertainty, commutability | Monitoring long-term method performance, detecting drift |
| Stable Control Materials | Daily system suitability testing | Homogeneity, stability, matrix matching | Monitoring precision, detecting special cause variation |
| Grade-Appropriate Solvents & Reagents | Experimental procedures | Specification compliance, lot-to-lot consistency | Controlling background noise, minimizing reagent-induced variation |
| Column/Stationary Phase Lots | Separation techniques | Performance qualification, retention characteristics | Managing method transfer challenges, lifecycle management |
Proper management of these critical reagents includes establishing rigorous qualification protocols, maintaining comprehensive documentation, and conducting bridging studies when lots change. These practices directly support the Check phase by ensuring that observed variation stems from the process under investigation rather than from material inconsistencies [70].
Integrated PDCA-Experimental Workflow
For complex variation analysis, the PDCA cycle integrates with structured experimental approaches. The following diagram illustrates this integrated workflow:
This integrated approach enables researchers to systematically investigate complex systems, identify significant sources of variation, and implement targeted improvements. The structured nature of PDCA ensures that process changes are based on empirical evidence rather than assumptions, leading to more robust and reliable experimental outcomes.
Managing Lurking Variables and Unexplained Variation
FAQs on Lurking Variables and Experimental Variation
1. What is the difference between a lurking variable and a confounding variable?
Both lurking and confounding variables are extraneous variables that are related to both your explanatory (independent) and response (dependent) variables, potentially creating a false impression of a causal relationship [75]. The key difference lies in whether the variable was measured or recorded in the study.
- Confounding Variable: This is an extraneous variable that has been measured, assessed, or recorded by the researchers [75]. Because it is known and measured, its effects can be accounted for during the experimental design or statistical analysis.
- Lurking Variable: This is a confounding variable that has not been measured, assessed, or recorded [75]. Since it is unknown or unmeasured, it can introduce bias without your knowledge, making it a more significant threat to the validity of your conclusions.
The relationship between these terms is summarized in the table below.
| Variable Type | Associated with Response Variable? | Associated with Explanatory Variable? | Measured or Observed? |
|---|---|---|---|
| Extraneous Variable | Yes [75] | No | Not Applicable |
| Confounding Variable | Yes [75] | Yes [75] | Yes [75] |
| Lurking Variable | Yes [75] | Yes [75] | No [75] |
Table 1: Classification and characteristics of different variable types that can impact experimental results.
2. What are the three key principles of experimental design used to control for lurking variables and unexplained variation?
The three fundamental principles are Randomization, Blocking, and Replication [76].
- Randomization: This involves randomly assigning the order of experimental trials or runs. It helps average out the effects of uncontrolled (lurking) variables over all treatments, preventing systematic bias [76] [77]. For example, if you don't randomize, the effect of a lurking variable like ambient temperature could be mistaken for the effect of your treatment.
- Blocking: This is a technique used to reduce variability from known nuisance factors that are not the primary interest of the study. You divide the experiment into homogeneous groups (blocks), and all treatments are applied within each block. This allows you to remove the variability between blocks from the experimental error [76] [77]. Common blocking factors include different batches of raw material, different days, or different operators [77].
- Replication: This means repeating the same experimental treatment on multiple independent experimental units. It enables you to estimate the experimental error, which is the natural, unexplained variation in your system [76]. Without replication, you cannot determine if the difference between treatments is due to the treatment itself or just random variation.
3. What is a systematic troubleshooting process for experiments with unexpected results?
A structured approach to troubleshooting is critical for efficiency. The following step-by-step guide, adapted from common laboratory practices, provides a logical framework [78]:
- Identify the Problem: Clearly define what went wrong without assuming the cause (e.g., "no PCR product detected" instead of "the primers are bad") [78].
- List All Possible Explanations: Brainstorm every potential cause, from the obvious (e.g., reagent concentrations, equipment settings) to the less obvious (e.g., sample degradation, technician error) [78].
- Collect Data: Review your data and controls. Check if equipment is functioning, reagents are stored correctly and are not expired, and that the protocol was followed exactly [78] [79].
- Eliminate Explanations: Based on the data collected, rule out causes that are not supported. For example, if positive controls worked, the core reagents are likely not the issue [78].
- Check with Experimentation: Design and run a new, targeted experiment to test the remaining possible explanations. It is critical to change only one variable at a time to correctly identify the true cause [78] [79].
- Identify the Cause: After analyzing the results of your targeted experiments, you should be able to identify the root cause and take steps to fix it [78].
4. How can I proactively manage variation when developing a new analytical method in drug development?
The Quality by Design (QbD) framework, guided by ICH guidelines, is a systematic, proactive approach for this purpose [80]. It emphasizes building quality into the method from the start rather than relying only on end-product testing. Key steps include:
- Define a Quality Target Product Profile (QTPP): This is a prospective summary of the quality characteristics your method needs to have [80].
- Identify Critical Quality Attributes (CQAs): These are the measurable properties and performance characteristics of your method (e.g., accuracy, precision, linearity) that must be controlled to ensure quality [80].
- Perform Risk Assessment: Use tools like Failure Mode and Effects Analysis (FMEA) to identify which material attributes and process parameters (e.g., pH, temperature, reagent purity) can potentially impact your CQAs [80].
- Design of Experiments (DoE): Use statistical DoE to systematically characterize the method and understand the relationship between the key factors you identified and your CQAs. This helps you establish a "design space," which is the range of parameters where the method performs robustly [80] [81].
- Develop a Control Strategy: Implement a set of controls, such as standard operating procedures (SOPs) and in-process checks, to ensure your method remains within the design space during routine use [80].
Troubleshooting Guides
This workflow provides a logical path to isolate the root cause of high variation or unexpected results in your data.
Diagram 1: A diagnostic workflow for identifying the source of unexplained variation in experiments.
Guide 2: Systematic Protocol Troubleshooting
When your experimental protocol fails (e.g., no signal, high background noise), follow this iterative process to identify the issue efficiently [78] [79].
Diagram 2: A cyclical process for troubleshooting failed experimental protocols.
Research Reagent Solutions
This table lists essential materials and their functions in the context of managing variation and validating methods.
| Item | Function | Application in Variation Control |
|---|---|---|
| Reference Standards | Well-characterized materials used to calibrate equipment and determine the accuracy (bias) of an analytical method [81]. | Serves as a benchmark to ensure measurements are correct and consistent across different batches and instruments. |
| Positive Controls | Samples that are known to produce a positive result. Used to verify that the experimental system is working correctly [79]. | Helps distinguish between a true negative result and a protocol failure. A failed positive control indicates a problem with the method itself. |
| Negative Controls | Samples that are known to produce a negative result (e.g., no template in PCR, no primary antibody in staining) [79]. | Used to identify background signal or contamination, ensuring that the measured effect is actually due to the treatment. |
| Placebos | Inactive substances that resemble the actual drug product but contain no active pharmaceutical ingredient (API) [82]. | In clinical trials, they are used as a control to account for the psychological and physiological effects of receiving a treatment, isolating the effect of the API. |
| Premade Master Mixes | Optimized, standardized mixtures of reagents for common reactions like PCR [78]. | Reduces operator-to-operator variation and pipetting errors, enhancing the reproducibility and precision of the assay. |
Proving Rigor: Validation Protocols and Comparative Study Designs
Designing a Comparison of Methods Experiment
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q: What is the main advantage of using a Completely Randomized Design (CRD) in quantitative genetics research? A: The main advantage of using a CRD is its simplicity and ease of implementation, making it suitable for experiments with a small number of treatments and homogeneous experimental material [83].
Q: How do I choose between a Completely Randomized Design (CRD) and a Randomized Complete Block (RCB) design? A: The choice depends on the experimental conditions and research question. If the experimental material is heterogeneous or there are obvious sources of variation, an RCB design is more suitable as it groups experimental units into blocks to reduce variation and improve precision [83].
Q: My assay shows a complete lack of an assay window. What should I check first? A: First, verify your instrument was set up properly, as this is the most common reason for no assay window. For TR-FRET assays, ensure you are using the correct emission filters, as the emission filter choice can make or break the assay. Consult your instrument setup guides for proper configuration [84].
Q: Why might I get different EC50/IC50 values for the same compound between different labs? A: Differences in stock solution preparation are the primary reason for EC50/IC50 variations between labs. Even with the same compound, differences in preparation at the 1 mM stock concentration can lead to significant variability in results [84].
Q: What are the major sources of variability I should consider in biological experiments? A: Sources of variability are broadly divided into biological variability (due to subjects, organisms, biological samples) and technical variability (due to measurement, instrumentation, sample preparation). A key study found that for human tissue biopsies, the greatest source of variability was often different regions of the same patient's biopsy, followed by inter-patient variation (SNP noise). Experimental variation (RNA, cDNA, cRNA, or GeneChip) was minor in comparison [1].
Q: How can I improve the robustness of my assay data? A: Use the Z'-factor to assess assay robustness, which considers both the assay window size and the data variability (standard deviation). An assay with a large window but high noise may be less robust than one with a smaller window and low noise. Assays with Z'-factor > 0.5 are generally considered suitable for screening [84].
Troubleshooting Common Experimental Problems
Problem: No assay window in a TR-FRET assay.
- Potential Cause: Incorrect instrument setup or emission filters.
- Solution:
- Refer to instrument setup guides for your specific model.
- Verify the emission filters are exactly those recommended for TR-FRET assays.
- Test your microplate reader's TR-FRET setup using reagents you have on hand before running the actual assay [84].
Problem: High variability in gene expression profiling data.
- Potential Cause: Tissue heterogeneity and inter-individual variation (SNP noise) are major contributors, often more than technical experimental error.
- Solution:
- Consider pre-profile mixing of patient cRNA samples to effectively normalize both intra- and inter-patient sources of variation.
- This mixing approach can retain a high degree of specificity while reducing unwanted variability [1].
Problem: Inconsistent results between replicate experiments.
- Potential Cause: Inadequate replication or failure to account for known sources of variation.
- Solution:
- Ensure sufficient replication to reduce the impact of random error.
- Use blocking (e.g., Randomized Complete Block Design) to group experimental units and account for spatial or temporal variation.
- Apply randomization to minimize bias and evenly distribute confounding variables [83].
Problem: Drug candidate shows high potency in vitro but fails in clinical development due to efficacy/toxicity balance.
- Potential Cause: Over-emphasis on potency/specificity (Structure-Activity-Relationship) without considering tissue exposure/selectivity (Structure-Tissue exposure/selectivity-Relationship).
- Solution:
- Adopt a Structure-Tissue exposure/selectivity-Activity Relationship (STAR) framework during drug optimization.
- Classify drug candidates based on both potency/selectivity AND tissue exposure/selectivity to better predict clinical dose, efficacy, and toxicity balance [85].
Data derived from 56 human muscle biopsy RNAs and 36 murine RNAs hybridized to Affymetrix arrays. [1]
| Source of Variability | Relative Contribution | Notes / Examples |
|---|---|---|
| Tissue Heterogeneity (different regions of same biopsy) | Greatest source in human muscle studies | Reflects variation in cell type content even in a relatively homogeneous tissue. |
| Inter-Patient Variation (SNP noise) | Very High | Polymorphic variation between unrelated individuals. |
| Experimental Variation (RNA, cDNA, cRNA, GeneChip) | Minor | Technical replication was not a significant source of unwanted variability. |
Table 2: Comparison of Statistical Methods for Quantifying Variability
Based on case studies analyzing *Listeria monocytogenes growth and inactivation.* [86]
| Method | Key Principle | Advantages | Limitations / Considerations |
|---|---|---|---|
| Simplified Algebraic Method | Uses algebraic equations to estimate variance components. | Relatively easy to use; good for initial assessments. | Overestimates between-strain and within-strain variability due to propagation of experimental error; results are biased. |
| Mixed-Effects Models | Incorporates both fixed effects (treatments) and random effects (experimental units). | Robust; provides unbiased estimates; easier to implement than Bayesian models. | Requires understanding of model structure and random effects specification. |
| Multilevel Bayesian Models | Uses Bayesian probability to estimate parameters and uncertainty. | High precision and flexibility; provides unbiased estimates; incorporates prior knowledge. | High complexity; computationally intensive. |
Table 3: STAR Classification for Drug Candidate Optimization
The Structure-Tissue exposure/selectivity-Activity Relationship (STAR) framework improves prediction of clinical success. [85]
| STAR Class | Specificity/Potency | Tissue Exposure/Selectivity | Required Clinical Dose | Clinical Efficacy/Toxicity Balance & Success |
|---|---|---|---|---|
| Class I | High | High | Low | Superior efficacy/safety; high success rate. |
| Class II | High | Low | High | Achieves efficacy but with high toxicity; evaluate cautiously. |
| Class III | Low (Adequate) | High | Low | Achieves efficacy with manageable toxicity; often overlooked. |
| Class IV | Low | Low | N/A | Inadequate efficacy/safety; should be terminated early. |
Experimental Protocols
Protocol 1: Implementing a Randomized Complete Block (RCB) Design
Application: Suitable for experiments with a larger number of treatments, heterogeneous experimental material, or obvious sources of variation [83].
Methodology:
- Group Experimental Units: Divide all experimental units (e.g., plots, animals, cell culture plates) into blocks. Each block should contain units that are as homogeneous as possible. The goal is to group known sources of variation (e.g., location in a growth chamber, different days) within a block.
- Assign Treatments: Within each block, randomly assign all treatments to the experimental units. This randomization must be performed independently for each block.
- Data Collection: Measure the response variable for each experimental unit.
- Statistical Analysis: Analyze data using an Analysis of Variance (ANOVA) model that includes both the treatment effect and the block effect. A mixed-effects model can be used, represented as: ( Y_{ij} = \mu + \tau_i + u_j + \epsilon_{ij} ) where ( Y_{ij} ) is the response, ( \mu ) is the overall mean, ( \tau_i ) is the fixed effect of the i-th treatment, ( u_j ) is the random effect of the j-th block, and ( \epsilon_{ij} ) is the random error [83].
Protocol 2: Mixed cRNA Sample Preparation for Expression Profiling
Application: Normalizing intra- and inter-patient variability in gene expression studies using Affymetrix GeneChips [1].
Methodology:
- Individual Sample Preparation: Isolate RNA from each individual biological sample (e.g., different regions of a tissue biopsy, different patients).
- Convert to cRNA: Independently convert each RNA sample to double-stranded cDNA, and then to biotinylated cRNA.
- Create Mixed Pools: Combine equal amounts of cRNA from multiple individual samples into a single, mixed cRNA pool. Samples should be matched for relevant variables (e.g., disease, age, sex).
- Hybridize to Array: Hybridize the mixed cRNA pool to the GeneChip microarray.
- Data Analysis: Process and analyze the hybridized array using standard software (e.g., Affymetrix Microarray Suite). This approach retains a high degree of specificity while effectively reducing variability from tissue heterogeneity and inter-patient genetic differences [1].
Protocol 3: Assessing Assay Robustness with Z'-Factor
Application: Determining the suitability of an assay (e.g., TR-FRET, Z'-LYTE) for high-throughput screening [84].
Methodology:
- Run Controls: Perform the assay using positive and negative controls that represent the maximum and minimum possible signals (e.g., 0% inhibition and 100% inhibition). Use a sufficient number of replicates (e.g., n≥16 per control is recommended).
- Calculate Means and Standard Deviations: For both the positive control (max signal, ( \mu_p ), ( \sigma_p )) and the negative control (min signal, ( \mu_n ), ( \sigma_n )).
Compute Z'-Factor: Use the following formula: ( Z' = 1 - \frac{3\sigma_p + 3\sigma_n}{|\mu_p - \mu_n|} )
Interpret Results:
- ( Z' > 0.5 ): An excellent assay suitable for screening.
- ( 0 < Z' \leq 0.5 ): A marginal assay that may be used for screening but could benefit from optimization.
- ( Z' \leq 0 ): Assay is not suitable for screening. Investigate sources of high variability or a small assay window [84].
Experimental Workflow and Relationship Visualizations
Experimental Design Workflow
Hierarchy of Variability Sources
STAR Framework for Drug Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Variation Analysis Experiments
| Item / Reagent | Function / Application | Key Considerations |
|---|---|---|
| Affymetrix GeneChip Microarrays | High-throughput gene expression profiling. Contains 30-40 redundant oligonucleotide probes per gene for specificity. | Standardized factory synthesis allows for databasing and cross-lab comparison. Newer generations (e.g., U74Av2) show high reproducibility (R² > 0.979) [1]. |
| LanthaScreen TR-FRET Assays (Terbium/Europium) | Time-Resolved Fluorescence Resonance Energy Transfer assays for studying biomolecular interactions (e.g., kinase activity). | Critical: Use exact emission filters recommended for your instrument. The acceptor/donor emission ratio corrects for pipetting variance and reagent lot variability [84]. |
| Z'-LYTE Kinase Assay Kit | Fluorescent, coupled-enzyme assay for measuring kinase activity and inhibitor screening. | Output is a blue/green ratio. The 100% phosphorylated control should give the minimum ratio, and the cleaved substrate (0% phosphorylation) the maximum ratio [84]. |
Mixed-Effects Model Software (e.g., R lme4, Python statsmodels) |
Statistical analysis to partition variability into fixed effects (treatments) and random effects (blocks, subjects, strains). | Provides unbiased estimates of variability components (between-strain, within-strain, experimental). More robust and easier to implement than complex Bayesian models for many applications [86]. |
| Biotinylated cRNA | Target for hybridization to oligonucleotide microarrays. | Quality control is essential: ensure sufficient amplification and check post-hybridization scaling factors. Pre-profile mixing of cRNA from multiple samples can normalize inter-patient variability [1]. |
Frequently Asked Questions (FAQs)
Q1: What is the primary goal of linearity validation in an analytical method?
A: The goal of linearity validation is to demonstrate that your analytical method produces results that are directly proportional to the concentration of the analyte across a specified range. This is a cornerstone parameter ensuring reliable quantification. It involves establishing a calibration curve and verifying that the method's response is linear, typically confirmed by a combination of statistical metrics and visual inspection of residuals [87].
Q2: Why is a high correlation coefficient (r²) alone insufficient to prove linearity?
A: A high r² value (e.g., >0.995) indicates a strong correlation but does not guarantee a good model fit. It is possible to have a high r² while the data exhibits patterns like non-linearity, outliers, or heteroscedasticity. Therefore, it is essential to also visually inspect residual plots. A random scatter of residuals around zero suggests a good fit, while a discernible pattern indicates a problem with the model [87] [88].
Q3: What is bias in the context of regression analysis and method validation?
A: In statistics, bias refers to the difference between an estimator's expected value and the true value of the parameter being estimated. In method validation, it often manifests as systematic error where results are consistently higher or lower than the true value. It is an objective property of an estimator, distinct from inaccuracy, which might also include random error [89].
Q4: How can I determine if the bias in my method is acceptable?
A: Bias should be evaluated against predefined acceptance criteria, which are often derived from regulatory requirements or proficiency testing schemes. For instance, in US laboratories, CLIA regulations define allowable total error. The estimated bias from a comparison of methods experiment should fall within these acceptable limits to ensure the method's accuracy is sufficient for its intended use [90].
Q5: What is the difference between Bland-Altman analysis and regression analysis for method comparison?
A:
- Regression Analysis is used to model the relationship between the test and comparison methods. It provides estimates of proportional error (slope) and constant error (intercept), allowing for the calculation of systematic error at any decision level [90].
- Bland-Altman Analysis plots the differences between the two methods against their averages. It primarily emphasizes random error between methods and provides an average estimate of bias. However, this estimate of bias is only reliable at the mean of the data if proportional error is present [90].
Regression is generally preferred when quantitative estimates of different error components are needed across the measuring range.
Troubleshooting Guides
Issue 1: Poor Linearity in Calibration Curve
Problem: The calibration curve shows a low r² value or a clear non-random pattern in the residual plot.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Inappropriate concentration range | Review the chosen range. Is it too wide, causing detector saturation, or too narrow? | Re-design the calibration standards to bracket the expected sample values evenly, typically from 50% to 150% of the target concentration [87]. |
| Matrix effects | Check if standards are prepared in a simple solvent that does not match the complex sample matrix. | Prepare calibration standards in a blank matrix or use a standard addition method to account for matrix interference [87]. |
| Instrumental issues | Look for signs of detector saturation at high concentrations or insufficient sensitivity at low concentrations. | Check the instrument's linear dynamic range and optimize settings. You may need to dilute high-end samples or concentrate low-end ones. |
Issue 2: High Bias in Method Comparison
Problem: The new method shows a consistent, significant difference (bias) from the comparison method.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Calibration error | Analyze primary standards alongside commercial calibrators to check for disagreement. | Resolve any calibration discrepancies before proceeding. Ensure the method is calibrated as intended for routine use [90]. |
| Interference | Perform a specific interference experiment by adding potential interferents to samples. | Identify and remove the source of interference, or incorporate a sample clean-up step (e.g., solid-phase extraction) into the method [87] [90]. |
| Incorrect comparison method | Evaluate if the "old" method used for comparison itself has known biases. | Whenever possible, use a reference method that is known to be free of significant systematic errors for the comparison [90]. |
Issue 3: Non-Random Patterns in Residual Plots
Problem: The plot of residuals versus predicted values or concentration shows a systematic pattern (e.g., a curve or funnel shape).
| Pattern Observed | Interpretation | Remedial Action |
|---|---|---|
| U-shaped or inverted U-shaped curve | Suggests the functional form of the model is incorrect; the true relationship may be non-linear [88]. | Consider using a non-linear regression model or transforming the data (e.g., logarithmic transformation). |
| Funnel shape (increasing spread with concentration) | Indicates heteroscedasticity - non-constant variance of errors [88]. | Use a weighted regression model instead of ordinary least squares, where points with higher variance are given less weight. |
| A clear trend (upward or downward slope) | Suggests the model is missing a key variable or there is drift in the instrument over time [88]. | For drift, randomize the order of sample analysis. If a variable is missing, re-evaluate the model. |
Experimental Protocols & Data Presentation
Protocol 1: Validating Method Linearity
Objective: To demonstrate that the analytical procedure yields test results proportional to analyte concentration within a specified range.
Methodology:
- Preparation of Standards: Prepare a minimum of five calibration standards, independently, spanning the intended range (e.g., 50%, 75%, 100%, 125%, 150% of the target concentration) [87].
- Analysis: Analyze each concentration level in triplicate, in a randomized run order to eliminate systematic bias [87].
- Data Analysis:
- Plot the mean response against the concentration.
- Perform linear regression to obtain the correlation coefficient (r²), slope, and y-intercept.
- Generate a plot of residuals (difference between observed and predicted values) versus concentration.
Acceptance Criteria:
- The correlation coefficient (r²) should typically exceed 0.995 [87].
- The residual plot should show random scatter of points around zero with no obvious patterns [87].
Protocol 2: Estimating Bias via Method Comparison
Objective: To estimate the systematic error (bias) of a new method by comparing it to a reference or established method.
Methodology:
- Sample Selection: Analyze at least 40 patient samples covering the entire reportable range using both the new (test) method and the comparison method [90].
- Data Analysis:
- Use Deming regression or a similar model that accounts for error in both methods to calculate the slope and intercept [90].
- The y-intercept provides an estimate of constant bias.
- The slope provides an estimate of proportional bias (a slope ≠ 1 indicates proportional error).
- Calculate the overall bias at critical medical decision levels using the regression equation:
Bias = (Slope * Xc) + Intercept - Xc, whereXcis the decision level concentration.
Data Presentation Table: The following table summarizes key parameters and their acceptance criteria for a hypothetical glucose assay.
| Performance Characteristic | Experimental Result | Acceptance Criterion | Status |
|---|---|---|---|
| Linearity (r²) | 0.998 | > 0.995 | Pass |
| Residual Plot | Random scatter | No systematic pattern | Pass |
| Constant Bias (Intercept) | 0.15 mg/dL | ± 0.5 mg/dL | Pass |
| Proportional Bias (Slope) | 0.985 | 0.98 - 1.02 | Pass |
| Bias at 100 mg/dL | -1.35 mg/dL | < ± 5 mg/dL | Pass |
Workflow Visualization
Linearity Validation and Bias Assessment Workflow
Troubleshooting Non-Linear Regression
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in Validation |
|---|---|
| Certified Reference Materials | Provides a definitive value for the analyte, used to establish accuracy and calibrate the method [90]. |
| Blank Matrix | The biological or chemical sample without the analyte. Used to prepare calibration standards to mimic the sample and account for matrix effects [87]. |
| Quality Control Materials | Stable materials with known (or assigned) concentrations. Used in replication experiments to determine precision (imprecision) and for ongoing quality control [90]. |
| Primary Standards | Highly purified compounds used to verify the accuracy of commercial calibrators and prepare master calibration curves [90]. |
| Interference Check Solutions | Solutions containing known potential interferents. Used to test the method's specificity by spiking into samples and observing the bias [90]. |
Randomized Controlled Trials (RCTs) vs. Non-Randomized Designs
FAQs: Core Concepts and Design Selection
FAQ 1: What is the fundamental difference between an RCT and a non-randomized study?
The core difference lies in how participants are assigned to intervention groups.
- Randomized Controlled Trials (RCTs) use random assignment to allocate participants to different interventions. This process balances both known and unknown participant characteristics (e.g., age, disease severity, genetic background) across the groups, minimizing selection bias and providing a rigorous basis for establishing cause-effect relationships [91] [92].
- Non-Randomized Studies of Interventions (NRSIs) allocate participants to comparison groups through a non-random process, such as clinician choice, patient preference, or administrative decisions. This makes them prone to selection bias and confounding, where underlying differences between the groups can influence the observed outcomes [93] [92].
FAQ 2: When is it appropriate to use a non-randomized design instead of an RCT?
Non-randomized designs are crucial in situations where RCTs are not feasible, ethical, or sufficient. The Cochrane Handbook outlines key justifications for their use [92]:
- To evaluate interventions that cannot be randomized. This includes population-level public health policies (e.g., effects of legislation), interventions where participants have strong preferences, or surgical procedures that are difficult to randomize.
- To provide complementary evidence on intervention effects. NRSIs can address long-term outcomes, rare adverse events, different populations, or real-world delivery methods that may not be fully captured by existing RCTs.
- To inform the case for a future RCT by explicitly evaluating the available, albeit weaker, evidence.
FAQ 3: What are the main types of non-randomized study designs?
Non-randomized studies encompass a range of designs, each with distinct features and applications. The table below summarizes common types [94].
Table 1: Common Types of Non-Randomized Studies of Interventions (NRSIs)
| Type | Design | Brief Description | Control | Key Strengths | Key Weaknesses |
|---|---|---|---|---|---|
| Controlled Clinical Trial | Experimental | Participants are allocated to interventions non-randomly, but often follows a strict protocol. | Yes, Concurrent | Strict eligibility and follow-up; can measure incidence/risk. | Prone to selection bias and confounding. |
| Prospective Cohort Study | Observational | Recruits and follows participants over time, with groups defined by exposure status in routine practice. | Yes, Concurrent | Participants reflect routine practice; can demonstrate temporality. | Prone to confounding; expensive and time-consuming. |
| Retrospective Cohort Study | Observational | Identifies study participants historically based on their past exposure status. | Yes, Concurrent | Less expensive and time-consuming than prospective studies. | Prone to bias, confounding, and misclassification. |
| Case-Control Study | Observational | Compares participants with a specific outcome (cases) to those without it (controls). | Yes, Concurrent | Suitable for rare outcomes; cost-effective. | Prone to recall and selection bias; cannot measure incidence. |
| Before-After Study | Observational or Experimental | A single group is assessed before and after an intervention. | Historical (itself before) | Ease of enrollment. | Difficult to disentangle intervention effects from other temporal changes. |
| Case Series/Case Report | Observational | A description of outcomes in a single group or a single participant after an intervention. | No | Useful for rare diseases or new interventions. | Cannot infer association between intervention and outcome. |
FAQ 4: Why are RCTs considered the "gold standard" for establishing efficacy?
RCTs are considered the gold standard because the act of randomization balances participant characteristics (both observed and unobserved) between the groups. This allows researchers to attribute any differences in outcome to the study intervention rather than to pre-existing differences between participants, which is not possible with any other study design [91]. This minimizes bias and provides the strongest evidence for causal inference.
Troubleshooting Guides: Addressing Common Research Challenges
Challenge 1: My RCT and non-randomized study on the same intervention produced different results. Why?
This is a common issue, and a study called RCT-DUPLICATE demonstrated that much of the variation can be explained by specific emulation differences—aspects of the RCT that could not be perfectly replicated in the non-randomized, real-world evidence (RWE) study [95]. Key factors include:
- In-hospital start of treatment: Therapy initiation in a hospital setting (common in RCTs) is often not captured in claims data used for RWE studies [95].
- Discontinuation of baseline therapies: RCTs may require participants to discontinue certain medications at randomization, which does not reflect clinical practice [95].
- Delayed drug effects: Therapies with delayed onset may be missed in RWE studies due to shorter medication persistence in real-world settings compared to enforced adherence in RCTs [95].
- Outcome measurement: Differences in how outcomes are defined and measured (e.g., high-specificity adjudication in RCTs vs. low-specificity claims codes in RWE) can lead to variation [95].
Solution: When designing a non-randomized study to emulate an RCT, prospectively identify and document these potential emulation differences. A sensitivity analysis that accounts for these factors can help reconcile the results.
Challenge 2: How can I manage variation effectively in my experimental design?
Understanding and managing variation is fundamental to robust experimental design. The Biological Variation in Experimental Design and Analysis (BioVEDA) framework highlights that variation must be acknowledged and accounted for throughout the investigative process [96].
- During Experimental Design:
- Source Identification: Identify sources of variation (biological, environmental, experimental).
- Control Strategies: Use genetically similar model organisms, randomize treatments, and include control groups to minimize unwanted environmental and biological variation.
- Replication: Increase sample size to capture population-level variation and include technical replicates to account for measurement error.
- During Data Analysis:
- Visualization: Use appropriate graphs (e.g., histograms, individual data points) to represent variation visually.
- Summary Statistics: Calculate and report measures of variation (e.g., standard deviation, standard error).
- Statistical Analysis: Apply statistical tests that model and account for the identified sources of variation to draw valid conclusions [96].
Challenge 3: My non-randomized study is vulnerable to confounding. What can I do?
Confounding is a major limitation of non-randomized designs, but several methodological approaches can help mitigate it [92]:
- In the Design Phase:
- Matching: Select control participants who are similar to treated participants on key confounding variables (e.g., age, sex, disease severity).
- Restriction: Only include participants within a specific category of a confounder (e.g., only a specific age range).
- In the Analysis Phase:
- Stratification: Analyze the effect of the intervention within separate strata (subgroups) of the confounder.
- Multivariate Regression: Use statistical models to adjust for the effects of multiple confounders simultaneously.
- Propensity Score Methods: Create a single score that summarizes the probability of receiving the treatment given the confounders, and then match, stratify, or adjust for this score.
- Instrumental Variable Analysis: Use a variable that is related to the treatment assignment but not directly to the outcome to estimate the causal effect [92].
Challenge 4: Implementation fidelity is difficult to maintain in large-scale trials.
This is a common problem in both RCTs and non-randomized studies when scaling up. Solutions from public health and education research include:
- Become a "Learning Organization": Treat mediocre initial results as an opportunity to learn and improve implementation iteratively, rather than as a failure [97].
- Design for Ease: Ensure the intervention is easy for practitioners (e.g., teachers, nurses) to implement. If it feels difficult, time-consuming, or conflicts with existing protocols, adoption will be low [97].
- Establish Information Flows: Implement light-touch monitoring and accountability systems. Simply sharing implementation data (e.g., visit rates by district coaches) can create positive social influence and motivation [97].
Experimental Protocols and Methodologies
Protocol 1: Key Steps in Designing a Randomized Controlled Trial (RCT)
- Define Population and Interventions: Carefully select the study population, the interventions to be compared, and the primary outcomes of interest [91].
- Power Calculation: Calculate the number of participants needed to reliably detect a meaningful difference between groups, if one exists [91].
- Recruit and Randomize: Recruit eligible participants and use an automated randomization system with concealment (no prior knowledge of allocation) to assign them to intervention groups [91].
- Blinding: Whenever possible, implement blinding (single, double, or triple) so that participants, clinicians, and outcome assessors do not know the treatment assignment to minimize performance and detection bias [91].
- Follow-Up and Analyze: Conduct follow-up according to protocol. Analyze data by intention-to-treat (ITT), where participants are analyzed in the groups to which they were randomized, to maintain the benefits of randomization [91].
Protocol 2: Designing a Robust Prospective Cohort Study
- Define Exposure and Outcome: Clearly define the exposure (intervention) and the outcome(s) of interest. Ensure they are measurable in the chosen data source [94].
- Cohort Assembly: Identify and recruit a cohort of participants who are free of the outcome at the start of the study. Define study groups based on their exposure status in routine practice [94].
- Follow-Up Over Time: Follow participants prospectively over time to ascertain the development of outcomes in both exposed and unexposed groups [94].
- Data Collection on Confounders: Prospectively collect data on potential confounding variables to allow for statistical adjustment during analysis [94] [92].
- Analysis: Calculate and compare the incidence of outcomes between exposure groups. Use multivariate regression or other techniques to adjust for identified confounders.
Visualizing Study Design and Variation
The following diagram illustrates the logical decision pathway for selecting an appropriate study design based on the research context and goals, incorporating key concepts from the provided literature.
Decision Flow for RCT and Non-Randomized Study Design
This diagram outlines the core workflow for analyzing and accounting for different sources of variation in biological experiments, as conceptualized in the BioVEDA assessment [96].
Framework for Managing Variation in Experiments
The Scientist's Toolkit: Research Reagent Solutions
This table details key methodological "reagents" or tools essential for designing and analyzing studies on intervention effects.
Table 2: Essential Methodological Tools for Intervention Studies
| Tool / Solution | Function | Application Context |
|---|---|---|
| Randomization Sequence | Allocates participants to intervention groups by chance, minimizing selection bias and balancing known/unknown confounders. | The foundational element of an RCT [91]. |
| Power Analysis | Calculates the required sample size to detect a specified effect size with a given level of confidence, preventing underpowered studies with inconclusive results. | Used in the planning phase of both RCTs and NRSIs to ensure the study is adequately sized [98]. |
| Blinding (Masking) | Prevents knowledge of the treatment assignment from influencing participants, caregivers, or outcome assessors, reducing performance and detection bias. | Applied in RCTs and some controlled NRSIs where feasible [91]. |
| Propensity Score | A statistical tool that summarizes the probability of receiving the treatment given a set of observed covariates. Used to match or adjust for confounders in NRSIs. | Used in the analysis of NRSIs to simulate the balance achieved by randomization [92]. |
| Intention-to-Treat (ITT) Principle | Analyzes all participants in the groups to which they were originally randomized, regardless of what treatment they actually received, preserving the benefits of randomization. | The preferred analysis method for RCTs [91]. |
| CONSORT Statement | A set of evidence-based guidelines for reporting parallel-group randomized trials. Improves transparency and completeness of RCT publications. | Used when writing up and publishing the results of an RCT [91]. |
| Real-World Data (RWD) | Data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources (e.g., electronic health records, claims data). | The primary data source for many non-randomized studies generating real-world evidence (RWE) [95]. |
Assessing Internal and External Validity in Comparative Studies
Frequently Asked Questions (FAQs)
Q1: What is the core difference between internal and external validity?
- Internal Validity is the degree of confidence that a causal relationship exists between the treatment and the observed outcome. It asks: "Did the experimental treatment cause the change, or could something else be to blame?" A study with high internal validity uses rigorous design to ensure that no other factors are responsible for the effect [99] [100].
- External Validity is the extent to which the results of a study can be generalized to other contexts, including different people, settings, and times. It asks: "Would this finding hold true for other groups or in the real world?" [99] [100].
Q2: Why is there often a trade-off between internal and external validity?
There is a fundamental trade-off because the methods used to strengthen one often weaken the other [99].
- High Internal Validity is often achieved in controlled laboratory settings where variables are tightly managed and confounding factors are minimized. This control can make the experimental environment artificial.
- High External Validity is often sought in field studies or real-world settings that reflect natural conditions. However, these environments introduce more uncontrolled variables, making it harder to isolate a pure cause-and-effect relationship. A recommended solution is to first establish causality in a controlled setting (high internal validity) and then test if the results hold in a field experiment (assessing external validity) [99].
Q3: What is the role of random assignment in establishing validity?
Random assignment is a cornerstone for establishing internal validity. It involves assigning participants to treatment or control groups purely by chance [20] [101] [102].
- Function: It ensures that, on average, the groups are similar at the start of the experiment in all respects—both known and unknown. This minimizes selection bias and distributes confounding variables evenly across groups [20] [100].
- Outcome: Any systematic difference in outcomes between groups at the end of the experiment can therefore be more confidently attributed to the treatment effect rather than to pre-existing differences between participants [101].
Q4: How does blocking differ from randomization, and when should I use it?
While both are design techniques, they serve different purposes.
- Randomization deals with unknown sources of variation by randomly assigning subjects to treatments. It is a universal tool for reducing bias [102].
- Blocking deals with a known and influential source of variation. You group similar experimental units into "blocks" and then randomize treatments within each block. This allows you to isolate and remove the variability caused by the blocking factor, leading to a more precise estimate of the treatment effect [20] [102].
- When to Use: Use a randomized block design when you have a clear variable (e.g., age, gender, tumor stage, farm field gradient) that you know has a strong effect on the response variable [20].
Troubleshooting Guides
Guide 1: Diagnosing and Mitigating Threats to Internal Validity
If you are concerned that your observed effect might not be causal, consult the following table of common threats.
| Threat | Description | Diagnostic Check | Corrective/Mitigating Action |
|---|---|---|---|
| History | An external event occurs during the study that influences the outcome [99]. | Did any significant environmental or contextual changes coincide with the treatment? | Use a control group that experiences the same external events. Conduct the study in a controlled environment. |
| Maturation | Natural changes in participants over time (e.g., aging, fatigue) affect the outcome [99]. | Is the outcome variable one that could change predictably over the study's timeline? | Include a control group to account for these natural temporal trends. |
| Selection Bias | Systematic differences between treatment and control groups exist before the study begins [99]. | Compare baseline measurements of key characteristics between groups. | Implement random assignment instead of allowing self-selection or using non-random criteria [20] [100]. |
| Attrition | Participants drop out of the study in a non-random way, related to the treatment or outcome [99]. | Analyze the characteristics of participants who dropped out vs. those who completed. | Use statistical methods like intent-to-treat analysis. Collect reasons for dropout. |
| Testing | Taking a pre-test influences scores on a post-test [99]. | Are participants being exposed to the same assessment multiple times? | Use a control group that also takes both tests. Consider using different but equivalent forms for pre- and post-tests. |
| Instrumentation | The way the outcome is measured changes over the course of the study [99]. | Have the measurement tools, calibrations, or observers changed? | Standardize measurement protocols and tools. Train observers for consistency and use blinding. |
| Confounding | An unmeasured third variable is related to both the group assignment and the outcome [103]. | Is there a plausible variable that could be causing the observed effect? | During design: use randomization. During analysis: use statistical control (e.g., multiple regression). |
Guide 2: Diagnosing and Mitigating Threats to External Validity
If you are concerned that your findings may not generalize, consult this table.
| Threat | Description | Diagnostic Check | Corrective/Mitigating Action |
|---|---|---|---|
| Sampling Bias | The study sample is not representative of the target population of interest [99]. | How were participants recruited? Do their demographics match the target population? | Use random sampling from the target population. If not possible, use stratified sampling to ensure key subgroups are included [100]. |
| Hawthorne Effect | Participants change their behavior because they know they are being studied [99]. | Was the measurement process obtrusive? | Use blinding (single or double-blind designs) so participants are unaware of their group assignment or the study's primary hypothesis [20] [101]. |
| Interaction of Testing | Exposure to a pre-test sensitizes participants to the treatment, making the results generalize only to other pre-tested populations [99]. | Could the pre-test have made participants aware of what is being studied? | Use a design that does not rely on a pre-test, or include a group that receives the treatment without the pre-test. |
| Ecological Validity | The experimental setting, tasks, or materials are too artificial and do not reflect real-world conditions [100]. | How different is the lab environment from the natural context where the phenomenon occurs? | Conduct field experiments to replicate findings in a natural setting [99] [100]. |
Experimental Protocols for Validity Assessment
Protocol 1: Implementing a Randomized Block Design
This design is used to control for a known source of variability (a "nuisance variable") that could obscure the treatment effect, thereby increasing internal validity.
- Identify the Blocking Factor: Select a variable that is not of primary interest but is known to strongly influence the response variable (e.g., "Age Group," "Tumor Stage," "Manufacturing Batch").
- Form Blocks: Group experimental units that are homogeneous with respect to the blocking factor. For example, if blocking by "Batch," all units from Batch 1 form one block, all from Batch 2 form another, etc.
- Randomize Within Blocks: Randomly assign all treatments (including the control) to the units within each block. This ensures that each treatment is tested across all levels of the nuisance variable.
- Execute Experiment: Apply the treatments and measure the responses.
- Statistical Analysis: Analyze the data using a statistical model (e.g., ANOVA) that includes both the Block and Treatment as factors. This allows the variability due to the blocking factor to be separated from the variability due to the treatment, providing a more sensitive test of the treatment effect [20] [102].
Protocol 2: Harmonizing Measures for Integrative Data Analysis (IDA)
This protocol is for synthesizing data from multiple comparative studies (e.g., different clinical trials) to assess and enhance external validity. The goal is to create a common scale for an outcome measured differently across studies [104].
- Data Pooling: Collect raw, participant-level data from all available studies.
- Identify Bridging Items/Measures: Locify items or entire measures that are common across two or more of the studies. These "anchors" are essential for linking the different scales.
- Assess Dimensionality: Use psychometric analysis (e.g., Exploratory Factor Analysis) to confirm that all items from the different measures are assessing the same underlying construct (e.g., "depression").
- Test for Differential Item Functioning (DIF): Check that the items function the same way across different subpopulations (e.g., from different studies, age groups, or ethnicities). If an item shows DIF, it may need to be adjusted or excluded.
- Create Harmonized Scores: Apply Item Response Theory (IRT) modeling or a common factor model to calibrate all items onto a single, unified metric. This generates a comparable score for each participant, regardless of which original measure they completed [104].
- Validate and Analyze: Use the newly created harmonized scores to run the primary analysis (e.g., comparing treatment effects across the pooled dataset), which now has greater power and generalizability.
Visual Workflows for Validity Assessment
Diagram: Relationship Between Validity Types
The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key methodological "reagents"—conceptual tools and designs—essential for conducting valid comparative studies.
| Tool/Solution | Primary Function in Validity | Key Characteristics & Usage |
|---|---|---|
| Randomized Controlled Trial (RCT) | Establishes Internal Validity as the gold standard for causal inference [101]. | Participants are randomly assigned to treatment or control groups. Considered the most robust design for isolating treatment effects. |
| Blocking (in Randomized Block Design) | Increases precision and Internal Validity by controlling for a known nuisance variable [20] [102]. | Used when a specific, measurable factor (e.g., age, batch) is known to affect the outcome. Groups are formed by this factor before randomization. |
| Blinding (Single/Double) | Protects against biases (e.g., placebo effect, researcher bias) that threaten Internal Validity [20] [101]. | Single-blind: participants don't know their assignment. Double-blind: both participants and experimenters/evaluators are unaware. |
| Factorial Design | Allows efficient testing of multiple factors and their interactions, enhancing the informativeness of a study for external generalization [103] [102]. | Studies two or more factors simultaneously. Reveals if the effect of one factor depends on the level of another (e.g., Drug A works better for men than women). |
| Integrative Data Analysis (IDA) | Enhances External Validity by testing the consistency of effects across diverse studies and populations [104]. | A synthesis method that pools raw data from multiple studies. Uses statistical harmonization (e.g., IRT) to create comparable measures. |
| Cross-Validation | Assesses the External Validity of a statistical model by testing its predictive performance on new data [101]. | A technique where data is split into training and testing sets to evaluate how well the results of a model will generalize to an independent dataset. |
Establishing a Design Space and Analytical Control Strategies
Fundamental Concepts: FAQs
What is a Design Space? A Design Space is a scientifically established, multidimensional region of process parameters and material attributes that has been demonstrated to provide assurance of quality. Unlike a simple set of operating ranges, it accounts for interactions among variables, enabling true process understanding and optimization. Operating within an approved Design Space provides regulatory flexibility, as movement within this space does not typically require regulatory notification [105].
What is a Control Strategy? A Control Strategy is a planned set of controls, derived from current product and process understanding, that ensures process performance and product quality. These controls can include material attributes, in-process controls, process monitoring, and finished product specifications. The strategy is designed to manage the variability of the process and ensure it remains within the Design Space [106] [107].
How do Design Space and Control Strategy relate? The Design Space defines the relationship between Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs), identifying where acceptable product can be made. The Control Strategy provides the controls to ensure the process operates within the Design Space. The Control Strategy is what prevents the process from drifting into regions of limited knowledge or known failure [106].
What are common pitfalls when establishing a Design Space? A common misconception is that a Design Space eliminates the need for end-product testing; in reality, specifications remain in place. Practical challenges include the significant resource investment for multivariate studies, the difficulty in defining the space's edges (especially for continuous processes), and the organizational challenge of maintaining the knowledge over the product's lifecycle [105].
Troubleshooting Guides
Issue: The process consistently operates at the edge of the Design Space, risking failure.
- Potential Cause: The normal operating range (NOR) was not properly established as a subset of the Design Space where routine, robust manufacture occurs.
- Solution: Revisit the risk assessment and historical data to redefine the NOR. Strengthen the Control Strategy with more stringent in-process parametric controls or real-time monitoring (e.g., Process Analytical Technology - PAT) to provide early warning of drift [105] [106].
Issue: An analytical method is not "fit for purpose" across the entire Design Space.
- Potential Cause: The Analytical Target Profile (ATP) was developed based on a limited region of the Design Space and does not account for all potential process variations.
- Solution: The ATP must be defined to cover control requirements across the entirety of the Design Space. Use enhanced method development approaches that employ risk assessments to evaluate critical method variables, ensuring measurement uncertainty is controlled appropriately everywhere within the space [107].
Issue: A process change within the approved Design Space leads to an out-of-specification (OOS) result.
- Potential Cause: Inadequate model fit for the Design Space, or unaccounted-for scale-up effects that change the relationship between parameters and attributes.
- Solution: This indicates a need for Design Space lifecycle management. Data from the OOS event should be used to refine the model and understanding. Implement a continuous verification system and use regulatory mechanisms like Post-Approval Change Management Protocols (PACMP) to manage the knowledge update [105].
Experimental Protocols for Design Space Development
Protocol 1: Defining Criticality via Risk Assessment
Objective: To identify which material attributes and process parameters are critical and must be included in the Design Space [106].
- Identify Potential CQAs: Based on the Quality Target Product Profile (QTPP) and prior knowledge, list all physical, chemical, biological, or microbiological properties that could impact product safety or efficacy [107].
- Perform Initial Risk Assessment: Use a tool like a Fishbone (Ishikawa) diagram to brainstorm all input variables (process parameters, material attributes) that could impact the CQAs [105].
- Rank Risks Systematically: Conduct a Failure Mode and Effects Analysis (FMEA) to score each variable based on Severity, Probability, and Detectability. A high-risk ranking indicates a variable is likely critical and must be investigated further [105] [106].
- Iterate: The criticality of an attribute or parameter is not static. It should be re-evaluated as process knowledge increases throughout the product lifecycle [106].
Protocol 2: Mapping the Design Space using Design of Experiments (DoE)
Objective: To systematically explore the relationships between input variables (CPPs) and output responses (CQAs) to define the multidimensional region where quality is assured [105].
- Select Factors and Ranges: Choose the critical process parameters and material attributes identified in Protocol 1. Define a relevant range for each factor to be studied.
- Choose an Experimental Design: Select a structured, multivariate design such as a factorial or response surface design (e.g., Central Composite Design). This is efficient for capturing main effects and interactions [105].
- Execute the DoE: Run the experiments as per the design.
- Model the Data and Define the Space: Use statistical modeling (e.g., regression analysis, ANOVA) to build predictive equations linking inputs to outputs. The Design Space is the region where all CQA predictions simultaneously meet their required specifications [105] [108].
Visualization of Workflows and Relationships
Design Space Development Workflow
Relationship Between Knowledge, Design, and Control
The Scientist's Toolkit: Research Reagent Solutions
The following table details key components used in establishing a Design Space and Control Strategy [105] [107].
| Item/Component | Function in Experimentation |
|---|---|
| Design of Experiments (DoE) Software | Enables the planning of structured, multivariate experiments (e.g., factorial, response surface designs) to efficiently study multiple factors and their interactions simultaneously. |
| Risk Assessment Tools (e.g., FMEA software) | Provides a systematic framework for identifying, ranking, and prioritizing variables (process parameters, material attributes) that may impact product quality (CQAs). |
| Process Analytical Technology (PAT) | A system for real-time monitoring and control of Critical Process Parameters (CPPs) during manufacturing, enabling a dynamic Control Strategy (e.g., for real-time release). |
| Statistical Analysis Software (e.g., JMP, SPSS) | Used to analyze data from DoE studies; performs regression analysis, Analysis of Variance (ANOVA), and creates predictive models to map the Design Space. |
| Analytical Methods with ATP | Methods developed to meet a predefined Analytical Target Profile (ATP), ensuring they are "fit for purpose" to accurately measure CQAs across the entire Design Space. |
Conclusion
A well-conceived experimental design is not merely a preliminary step but the very foundation upon which reliable and actionable scientific knowledge is built. By systematically applying the principles outlined—from foundational concepts of replication and control to advanced methodologies like DoE and variance component analysis—researchers can transform variation from a source of noise into a quantifiable and understandable component of their system. This rigorous approach is paramount for building quality into pharmaceutical products, ensuring the reproducibility of preclinical research, and designing robust clinical trials. Future progress in biomedical research will increasingly depend on such strategic design frameworks to navigate the complexity of biological systems and deliver meaningful, trustworthy results that accelerate discovery and development.
References
- 1. Sources of variability and effect of experimental approach on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC65691/]
- 2. Lipidomic atlas of mammalian cell membranes reveals hierarchical ... [https://pubs.rsc.org/en/content/articlehtml/2021/sm/d0sm00404a]
- 3. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOorQsrM7VABD6VXgO68mD3d3novBbJPdFEFi9vJX2PUegGddvHyV]
- 4. 5 Steps to Follow for Troubleshooting Experiments [https://blog.edvotek.com/2022/06/21/5-steps-to-follow-for-troubleshooting-experiments/]
- 5. Types of Replicates: Technical vs. Biological [https://www.licorbio.com/blog/technical-and-biological-replicates]
- 6. 3 Independence & pseudoreplication [https://cambiotraining.github.io/stats-mixed-effects-models/materials/03-independence-psuedoreplication.html]
- 7. Optimal Allocation of Replicates for Measurement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5054083/]
- 8. The problem of pseudoreplication in neuroscientific studies [https://bmcneurosci.biomedcentral.com/articles/10.1186/1471-2202-11-5]
- 9. Pseudoreplication [https://web.ma.utexas.edu/users/mks/statmistakes/pseudorep.html]
- 10. A practical solution to pseudoreplication bias in single-cell ... [https://www.nature.com/articles/s41467-021-21038-1]
- 11. A Very Short List of Common Pitfalls in Research Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9477699/]
- 12. Better statistical reporting does not lead to statistical rigour [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105375/]
- 13. Experimental Unit - (AP Statistics) - Vocab, Definition, ... [https://fiveable.me/key-terms/ap-stats/experimental-unit]
- 14. Experimental unit | Definition & Example [https://www.britannica.com/science/experimental-unit]
- 15. Common Issues in Implementing Randomization and ... [http://onbiostatistics.blogspot.com/2022/04/common-issues-in-implementing.html]
- 16. it has typo "The experimental unit can, but does not have to ... [https://medium.com/@vijayvergia.ronak/it-has-typo-the-experimental-unit-can-but-does-not-have-to-be-the-same-as-the-randomization-and-cf5f63140321]
- 17. What are experimental units? [https://www.statsig.com/perspectives/experimental-units-explained]
- 18. Guidance on handling randomisation errors [https://pmc.ncbi.nlm.nih.gov/articles/PMC4509880/]
- 19. 7: Randomization Design Part I | STAT 502 [https://online.stat.psu.edu/stat502/lesson/7]
- 20. AP Statistics Experimental Design Explained (2025 Guide) [https://www.revisiondojo.com/blog/ap-statistics-experimental-design-explained-2025-guide]
- 21. What are Positive and Negative Controls? [https://scienceready.com.au/pages/positive-and-negative-controls?srsltid=AfmBOorvlOWNpHZ_rLs3Gsoyqqr2-2KgET8phMJEI3PtXZ3E_1zXLtf1]
- 22. Control Group Vs Experimental Group In Science [https://www.simplypsychology.org/control-and-experimental-group-differences.html]
- 23. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 24. Design of Experiments | Statistics Knowledge Portal [https://www.jmp.com/en/statistics-knowledge-portal/design-of-experiments]
- 25. Experimental Design [https://theminione.com/blog/2016/04/25/experimental-design/]
- 26. What Is Design of Experiments (DOE)? [https://asq.org/quality-resources/design-of-experiments?srsltid=AfmBOooWJc8veECrEvCAo_pISjpuGT2kfju5LBxEpb6rxQ0I99xGPvwR]
- 27. 10.5 Bonus section: DoE introduction for beginner [https://sisu.ut.ee/lcms_method_validation/105-bonus-section-doe-introduction-beginners/]
- 28. 5.3.3.4.6. Screening designs [https://www.itl.nist.gov/div898/handbook/pri/section3/pri3346.htm]
- 29. Screening Designs | Statistics Knowledge Portal [https://www.jmp.com/en/statistics-knowledge-portal/design-of-experiments/screening-designs]
- 30. Screening DOE: Efficient Factorial Designs for ... [https://www.6sigma.us/six-sigma-in-focus/screening-doe/]
- 31. Factorial Design Explained: Testing Multiple Factors [https://statisticsbyjim.com/basics/factorial-design/]
- 32. Sage Research Methods - Factorial Designs [https://methods.sagepub.com/ency/edvol/the-sage-encyclopedia-of-communication-research-methods/chpt/factorial-designs]
- 33. Chapter 7 Week 9 - Factorial ANOVA | 1014SCG Statistics - Lecture... [https://bookdown.org/mcbroom_j/Book/week-9-factorial-anova.html]
- 34. Factorial Designs — Main Effects, Interactions, and Multifactor ... [https://www.lastminutelecture.com/2025/09/chapter-11-factorial-designs-main-effects-interactions.html]
- 35. All Topics Factorial Design of Experiments [https://www.theopeneducator.com/doe/Factorial-Design-of-Experiments/all-topics-factorial-design-of-experiments]
- 36. Full Factorial : Comprehensive Guide for Optimal... Design [https://www.6sigma.us/six-sigma-in-focus/full-factorial-design/]
- 37. 7 Factorial Strategies: Boost Your Experiment Results Design [https://www.numberanalytics.com/blog/7-factorial-design-strategies-experiment-results]
- 38. Chapter 5 DoE for Troubleshooting and Improvement [https://bookdown.org/lawson/an_introduction_to_acceptance_sampling_and_spc_with_r26/doe-for-troubleshooting-and-improvement.html]
- 39. Variance components [https://analyse-it.com/docs/user-guide/measurement-systems-analysis/precision/variance-components]
- 40. Estimating Variance Components using LTRM Survey Data [https://www.umesc.usgs.gov/ltrmp/stats/variance.html]
- 41. Solved: Variance components [https://community.jmp.com/t5/Discussions/Variance-components/td-p/7904]
- 42. Why is the variance of my random effect negative? [https://stats.stackexchange.com/questions/19644/why-is-the-variance-of-my-random-effect-negative]
- 43. The Problem of Negative Estimates of Variance Components [https://projecteuclid.org/journals/annals-of-mathematical-statistics/volume-33/issue-1/The-Problem-of-Negative-Estimates-of-Variance-Components/10.1214/aoms/1177704731.full]
- 44. Variance Component Analysis [https://fionahorner.com/r-demos/variance-component-analysis/]
- 45. Design of Experiments for Formulation Development [https://www.pharmtech.com/view/design-experiments-formulation-development-0]
- 46. Quality by Design I: Application of Failure Mode Effect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3513475/]
- 47. Design of Experiments in Pharmaceutical Development [https://www.spcforexcel.com/knowledge/experimental-design-techniques/design-experiments-pharmaceutical-development/]
- 48. Best Practices For Implementing Design Of Experiments ... [https://enertherm-engineering.com/best-practices-for-implementing-design-of-experiments-doe-in-industrial-settings/]
- 49. DoE based failure mode effect analysis (FMEA) to ... [https://link.springer.com/article/10.1007/s42452-020-2890-1]
- 50. Confounding variables in statistics: How to identify and ... [https://www.statsig.com/perspectives/confounding-variables-statistics-identify-control]
- 51. Confounding Variables | Definition, Examples & Controls [https://www.scribbr.com/methodology/confounding-variables/]
- 52. Confounding: What it is and how to deal with it [https://www.sciencedirect.com/science/article/pii/S0085253815529748]
- 53. How to control confounding effects by statistical analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4017459/]
- 54. Strategies to Identify and Control Confounding Variables in ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5197954]
- 55. Randomization, blinding, and coding - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK305495/]
- 56. Selection of Control, Randomization, Blinding, and Allocation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6743387/]
- 57. Clinical Trial Randomization and Blinding Tools Directory ... [https://ccrps.org/clinical-research-blog/clinical-trial-randomization-and-blinding-tools-directory-and-reviews]
- 58. A Guide to Randomisation in Clinical Trials [https://www.quanticate.com/blog/randomisation-in-clinical-trials]
- 59. Navigating blinding challenges in complex intervention trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613531/]
- 60. 6 Ways to Protect the Blind in Clinical Trials [https://www.appliedclinicaltrialsonline.com/view/6-ways-protect-blind-clinical-trials]
- 61. SPIRIT 2025 statement: updated guideline for protocols of ... [https://www.nature.com/articles/s41591-025-03668-w]
- 62. Power (Statistics) - A Simple Introduction with Examples [https://www.spss-tutorials.com/power-in-statistics/]
- 63. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 64. & Statistical Sample Size Calculator Power Calculator [https://www.gigacalculator.com/calculators/power-sample-size-calculator.php]
- 65. Introduction to Power Analysis - OARC Stats [https://stats.oarc.ucla.edu/other/mult-pkg/seminars/intro-power/]
- 66. Sample Size Calculator [https://clincalc.com/stats/samplesize.aspx]
- 67. PDCA Cycle - What is the Plan-Do-Check-Act Cycle? | ASQ [https://asq.org/quality-resources/pdca-cycle]
- 68. What is the Plan-Do-Check-Act (PDCA) Cycle? [2025] • Asana [https://asana.com/resources/pdca-cycle]
- 69. Plan, Do, Check, Act (PDCA) — A Resource Guide [https://www.lean.org/lexicon-terms/pdca/]
- 70. The Effectiveness of the Plan-Do-Check-Act Cycle [https://businessmapping.com/bl160-the-effectiveness-of-the-plan-do-check-act-cycle.php]
- 71. Mastering the PDCA Cycle: The Key to Continuous Improvement in Product Management - Beyond the Backlog [https://beyondthebacklog.com/2025/03/20/the-pdca-cycle/]
- 72. What Is the PDCA Cycle? | Definition and Overview [https://www.productplan.com/glossary/pdca-cycle/]
- 73. 14.2 - Sources of variation - biostatistics.letgen.org [https://biostatistics.letgen.org/mikes-biostatistics-book/anova-designs-multiple-factors/sources-of-variation/]
- 74. Troubleshoot your experiment [https://amplitude.com/docs/feature-experiment/workflow/experiment-troubleshoot]
- 75. 6.3 Extraneous variables and variation in the response | Scientific... [https://bookdown.org/pkaldunn/Book/ExtraneousVariables.html]
- 76. Key Principles of Experimental Design [https://www.jmp.com/en/statistics-knowledge-portal/design-of-experiments/key-design-of-experiments-concepts/key-principles-of-experimental-design]
- 77. 4.1 - Blocking Scenarios | STAT 503 [https://online.stat.psu.edu/stat503/lesson/4/4.1]
- 78. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOopkkr6ZgJYF0qVyBlMWeyLn8ql5q6L2fjK1J3hUqQKxnfetCTvz]
- 79. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 80. Aspects and Implementation of Pharmaceutical Quality by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 81. Design of Experiments for Analytical Method Development ... [https://www.biopharminternational.com/view/design-experiments-analytical-method-development-and-validation]
- 82. The Art of Experimental Design: Techniques for ... [https://research-rebels.com/blogs/how-to-write-thesis/the-art-of-experimental-design-techniques-for-independent-variable-control]
- 83. Mastering Experimental in Quantitative Genetics Design [https://www.numberanalytics.com/blog/experimental-design-quantitative-genetics-guide]
- 84. Discovery Assays Support— Drug Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 85. Why 90% of clinical drug fails and how to improve it? development [https://pubmed.ncbi.nlm.nih.gov/35865092/]
- 86. Critical comparison of statistical methods for quantifying ... [https://www.sciencedirect.com/science/article/pii/S016816052200407X]
- 87. Ensuring Linearity in Method Validation - A Step-by- ... [https://altabrisagroup.com/linearity-in-method-validation/]
- 88. Regression validation [https://en.wikipedia.org/wiki/Regression_validation]
- 89. Bias of an estimator [https://en.wikipedia.org/wiki/Bias_of_an_estimator]
- 90. Basic Method Validation, 3rd Edition, FAQs [https://www.westgard.com/resources/resources/bmv3edfaqs.html]
- 91. Randomised controlled trials—the gold standard for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6235704/]
- 92. Including non-randomized studies on intervention effects [https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-24]
- 93. Nonrandomized control: understanding study design, ... [https://www.sciencedirect.com/science/article/pii/B9780323905091000540]
- 94. Table 1, Common types of nonrandomized studies of ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK584468/table/ch4.tab1/]
- 95. explain variation in results between Design ... differences randomized [https://pmc.ncbi.nlm.nih.gov/articles/PMC10370236/]
- 96. Development of the Biological Variation In Experimental And... Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC7371189/]
- 97. Six insights on implementation challenges at scale [https://www.wwhge.org/resources/six-insights-on-implementation-challenges-at-scale-and-how-to-fix-them/]
- 98. The Nonprofit Sector Has an RCT Problem [https://ssir.org/articles/entry/the-problem-with-randomized-controlled-trials]
- 99. Internal vs. External Validity | Understanding Differences & ... [https://www.scribbr.com/methodology/internal-vs-external-validity/]
- 100. Internal Validity vs External Validity in Research [https://mhcsandiego.com/blog/internal-validity-vs-external-validity-ensuring-research-accuracy/]
- 101. 10 Key Concepts in Experimental Design [https://www.statology.org/10-key-concepts-in-experimental-design/]
- 102. Design of experiments [https://en.wikipedia.org/wiki/Design_of_experiments]
- 103. Key Concepts for Design of Experiments [https://www.jmp.com/en/statistics-knowledge-portal/design-of-experiments/key-design-of-experiments-concepts]
- 104. Addressing Methodologic Challenges and Minimizing Threats ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5651214/]
- 105. : Regulatory Principles, Best Practices, and Trends Design Space [https://www.linkedin.com/pulse/design-space-regulatory-principles-best-practices-trends-r-fghyc]
- 106. PQLI Key Topics - Criticality, Design , and Space Control Strategy [https://link.springer.com/article/10.1007/s12247-008-9032-4]
- 107. Methods and Analytical : The Forgotten Interface? Control Strategies [https://pharmachitchat.wordpress.com/2015/05/22/analytical-methods-and-control-strategies-the-forgotten-interface/]
- 108. How thoughtful experimental design can empower ... [https://www.nature.com/articles/s41467-025-62616-x]