BlaR1 Sensor Inhibition: A Novel Strategy to Resensitize MRSA to β-Lactam Antibiotics
The global health crisis of antimicrobial resistance demands innovative therapeutic strategies, particularly against methicillin-resistant Staphylococcus aureus (MRSA).
BlaR1 Sensor Inhibition: A Novel Strategy to Resensitize MRSA to β-Lactam Antibiotics
Abstract
The global health crisis of antimicrobial resistance demands innovative therapeutic strategies, particularly against methicillin-resistant Staphylococcus aureus (MRSA). This article comprehensively reviews the groundbreaking approach of inhibiting the BlaR1 sensor protein to disarm bacterial resistance and restore the efficacy of conventional β-lactam antibiotics. We explore the foundational molecular biology of BlaR1-mediated signal transduction, analyze recent breakthroughs in inhibitor design and screening, address key challenges in drug optimization and delivery, and validate this strategy against other emerging therapies. Synthesizing current research and pre-clinical data, we provide a critical assessment for researchers and drug development professionals, highlighting BlaR1 inhibition as a promising pathway for developing effective antibiotic adjuvants to combat multidrug-resistant infections.
The BlaR1 Signaling Pathway: Decoding MRSA's β-Lactam Defense System
The Role of BlaR1 in Staphylococcal Resistance and the bla Operon
The bla operon is a key genetic determinant conferring inducible resistance to β-lactam antibiotics in Staphylococcus aureus, including methicillin-resistant S. aureus (MRSA) strains. This operon encodes three primary proteins: BlaR1, the sensor-signal transducer; BlaI, the gene repressor; and BlaZ, the PC1 β-lactamase [1]. In the absence of β-lactam antibiotics, BlaI represses the transcription of these genes by binding to operator regions within the operon. Upon exposure to β-lactams, BlaR1 senses the antibiotic and initiates a signal transduction cascade that culminates in the proteolytic degradation of BlaI, derepressing the operon and enabling the expression of resistance determinants [1] [2]. This sophisticated regulatory system allows MRSA to activate defense mechanisms only when challenged, conserving cellular resources. The following application note details the molecular mechanisms, experimental methodologies, and key reagents essential for investigating this system, with a particular focus on BlaR1 as a therapeutic target for resensitizing MRSA to β-lactam antibiotics.
Molecular Mechanism of BlaR1 Signaling
Signal Initiation: β-Lactam Sensing and Acylation
The resistance cascade begins when β-lactam antibiotics bind to the extracellular sensor domain of BlaR1. This domain shares structural homology with class D β-lactamases. The antibiotic acylates an active-site serine residue within this sensor domain, forming a stable acyl-enzyme complex [3] [4]. This acylation event is irreversible and enjoys a longevity that often exceeds the bacterial doubling time, meaning a single modification event can sustain the signal for an entire generation [1].
Signal Transduction: Conformational Activation
Acylation of the sensor domain triggers a series of conformational changes that propagate across the bacterial membrane. Recent cryo-EM structures of full-length BlaR1 reveal it forms a domain-swapped dimer [3]. The acylation event is proposed to competitively displace an extracellular loop from the sensor domain's active site, initiating a structural shift. This shift is transmitted through the transmembrane regions, ultimately affecting the conformation of the cytoplasmic zinc metalloprotease domain [3] [4]. This N-terminal metalloprotease domain contains the characteristic gluzincin motif (HExxH) and is embedded within the membrane, forming a hydrophilic chamber [3] [4].
Proteolytic Activation and Gene Derepression
The conformational change in the cytoplasmic domain activates its proteolytic function. Prior to activation, this domain undergoes autocleavage in cis between residues Ser283 and Phe284, an event that may contribute to its regulation [3]. The activated BlaR1 protease then directly cleaves the BlaI repressor [3]. BlaI is a DNA-binding protein that exists as a mixture of monomers and dimers at physiological concentrations and binds operator DNA primarily as a monomer [2]. Its cleavage releases the repression of the bla operon, allowing rapid transcription of blaZ (β-lactamase), blaR1, and blaI itself. The BlaZ β-lactamase then hydrolyzes the β-lactam antibiotic, conferring resistance [1].
Table 1: Key Molecular Events in BlaR1-Mediated Induction of Resistance
| Molecular Event | Key Participants | Outcome |
|---|---|---|
| β-Lactam Sensing | BlaR1 sensor domain, β-lactam antibiotic | Irreversible acylation of BlaR1 sensor |
| Signal Transduction | Transmembrane helices, BlaR1 dimer interface | Conformational change in cytoplasmic protease domain |
| Protease Activation | Zinc metalloprotease domain, autocleavage loop | Activation of proteolytic activity (autocleavage & BlaI cleavage) |
| Repressor Inactivation | BlaI repressor protein | Proteolytic degradation of BlaI |
| Gene Derepression | bla operator sequence (R1 & Z dyads) | Transcription of blaZ, blaR1, and blaI |
Phosphorylation as a Regulatory Layer
Beyond proteolytic activation, phosphorylation plays a critical role in BlaR1 signaling. Upon exposure to β-lactams, the cytoplasmic domain of BlaR1 is phosphorylated on at least one serine and one tyrosine residue [5]. Inhibition of this phosphorylation by synthetic kinase inhibitors abrogates the induction of resistance and can resensitize MRSA to β-lactam antibiotics, demonstrating that phosphorylation is essential for manifesting resistance [5].
System Reset and Recovery
Once the antibiotic challenge is removed, the system must reset. BlaR1 undergoes regulated fragmentation at specific sites in both the cytoplasmic and sensor domains [1]. This fragmentation, including the shedding of the acylated sensor domain into the medium, is proposed to be a turnover mechanism that allows the bacterium to recover from the induced state and return to a baseline level of vigilance [1] [6].
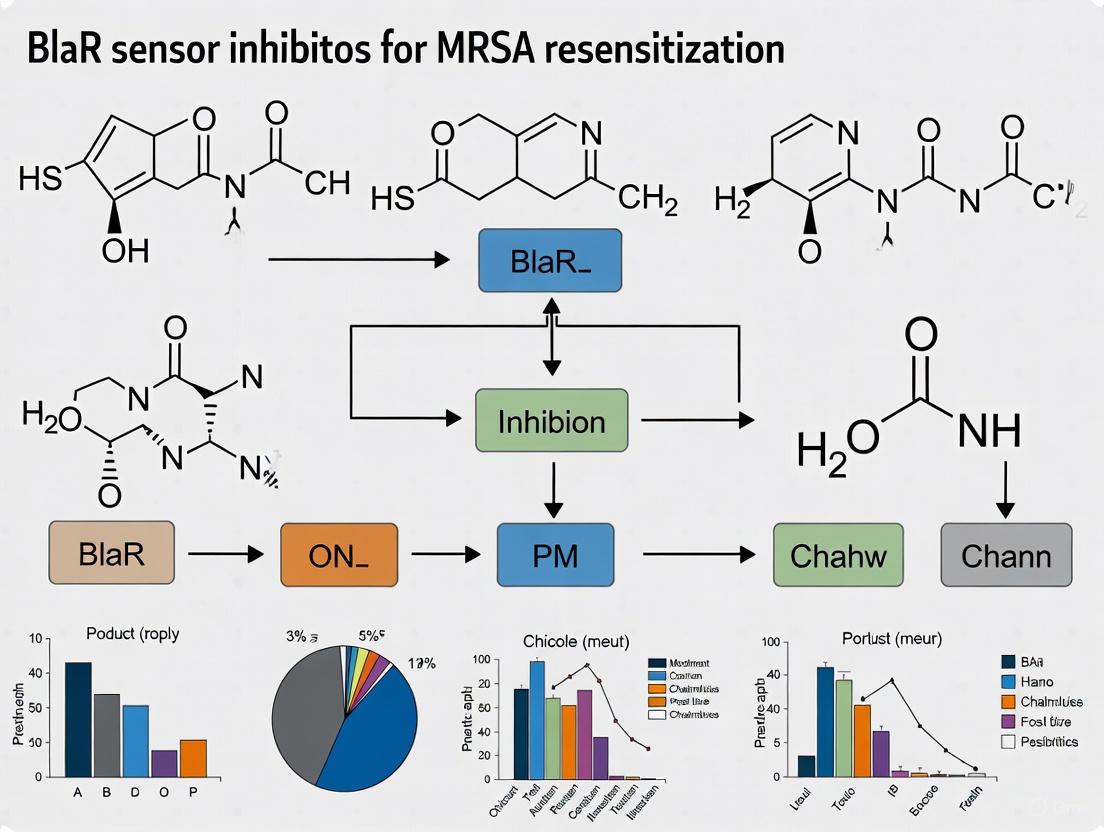
The diagram below summarizes the core signaling pathway of the BlaR1/BlaI system.
Quantitative Data on Key System Components
Understanding the biochemistry of the BlaR1/BlaI system requires knowledge of the molecular concentrations and binding affinities that govern its function.
Table 2: Quantitative Physicochemical Parameters of the BlaR1/BlaI System
| Component / Interaction | Measured Parameter | Value | Experimental Context |
|---|---|---|---|
| BlaI Repressor | In vivo concentration | 1.3 - 6.4 µM | S. aureus cells, exponential phase [2] |
| BlaI Monomer-Dimer Equilibrium | Dissociation Constant (Kd) | 1.61 ± 0.02 µM | Sedimentation equilibrium [2] |
| BlaI Binding to Full bla Operator | Monomer Kd (Kd1) | 0.45 ± 0.07 µM | Fluorescence anisotropy [2] |
| BlaI Binding to Z Dyad | Monomer Kd (Kd1) | 0.05 ± 0.04 µM | Fluorescence anisotropy [2] |
| BlaR1 Fragmentation | Timeframe for observation | Within 3 hours | Upon antibiotic exposure [1] |
| Kinase Inhibitor Efficacy | MIC reduction for oxacillin | 4 to 512-fold | In MRSA252, NRS123, NRS70 strains [5] |
Detailed Experimental Protocols
This section provides standardized protocols for key experiments investigating the BlaR1/BlaI system.
Protocol: Monitoring BlaR1 and BlaI Dynamics During Antibiotic Induction
This protocol is adapted from methodologies used to track the fate of BlaR1, BlaI, and β-lactamase in S. aureus upon antibiotic exposure [1].
Application: Used to study the time-dependent proteolytic events (BlaI degradation, BlaR1 fragmentation) and β-lactamase production that constitute the induction response.
Reagents:
- Bacterial Strains: MRSA strains (e.g., NRS128, NRS123, NRS70, MRSA252).
- Antibiotics: β-lactam antibiotics (e.g., Penicillin G, Ampicillin, Oxacillin, CBAP) prepared at sub-MIC concentrations.
- Growth Medium: Luria-Bertani (LB) broth.
- Lysis Buffer: 100 mM sodium phosphate (pH 7.5), 50 mM NaHCO₃, 1x EDTA-free protease inhibitor cocktail, 1 mM EDTA, 20 mM MgCl₂, DNase I (15 µg/ml), RNase A (15 µg/ml), lysostaphin (200 µg/ml).
- Antibodies: Rabbit polyclonal anti-BlaRS (recognizes BlaR1) and anti-BlaI.
Procedure:
- Culture and Induction: Grow 250 mL of S. aureus culture in LB at 37°C with shaking until the optical density at 625 nm (OD₆₂₅) reaches ~0.8 (exponential phase). Divide the culture into 30 mL aliquots. To each aliquot, add a sub-MIC concentration of a β-lactam antibiotic (e.g., 3.2x below MIC for penicillin, 6.4x below for CBAP). Maintain one aliquot as an uninduced control.
- Time-Course Sampling: Collect 5 mL samples from each culture at critical time points post-induction (e.g., 15 min, 30 min, 1 h, 3 h). Centrifuge samples at 3,200 × g for 30 min at 4°C to separate cell pellets from culture supernatants.
- Sample Preparation:
- Cell Pellet (Whole-Cell Extract): Resuspend pellets in Lysis Buffer and incubate at 37°C for 30 min. Quantify total protein concentration using an assay such as the BCA assay. Load 60-80 µg of total protein per lane for SDS-PAGE and subsequent Western blotting.
- Culture Supernatant: Assay immediately for extracellular β-lactamase activity using a nitrocefin hydrolysis assay or similar method. Supernatants can also be analyzed for the presence of the shed BlaR1 sensor domain.
- Analysis:
- Perform Western blot analysis on whole-cell extracts using anti-BlaI and anti-BlaR1 antibodies to monitor BlaI degradation and BlaR1 fragmentation over time.
- Measure β-lactamase activity in the supernatants spectrophotometrically to correlate repressor cleavage with resistance protein production.
Protocol: Assessing BlaR1 Phosphorylation and Inhibitor Effects
This protocol outlines the procedure for detecting BlaR1 phosphorylation and testing the efficacy of kinase inhibitors [5].
Application: Essential for validating the role of phosphorylation in signal transduction and for screening potential adjuvant compounds that resensitize MRSA to β-lactams.
Reagents:
- Bacterial Strains: S. aureus strains (e.g., NRS128, MRSA252).
- Inducer: CBAP (10 µg/mL).
- Kinase Inhibitors: Lead compounds (e.g., Inhibitors 10, 11, 12 from [5]).
- Lysis Buffer: (As in Protocol 4.1, supplemented with phosphatase inhibitors).
- Antibodies: Anti-phosphotyrosine, anti-phosphoserine, and anti-BlaR1.
Procedure:
- Culture and Treatment: Grow S. aureus cultures to the exponential phase. Treat cultures with:
- No additions (negative control).
- CBAP alone (positive control for induction).
- CBAP + varying concentrations of kinase inhibitor (e.g., 0.7 µg/mL, 7 µg/mL).
- Whole-Cell Extract Preparation: Harvest cells after a defined induction period (e.g., 1 h). Lyse cells using a suitable lysis buffer containing phosphatase inhibitors.
- Western Blot Analysis:
- Separate proteins by SDS-PAGE and transfer to a membrane.
- Probe the membrane with anti-phosphotyrosine and anti-phosphoserine antibodies to detect phosphorylation of BlaR1.
- Strip and re-probe the membrane with anti-BlaR1 antibody to confirm equal loading.
- Functional Validation (MIC Assay):
- Determine the Minimum Inhibitory Concentration (MIC) of oxacillin against the MRSA strain using the broth microdilution method in the presence and absence of the kinase inhibitor.
- A significant reduction (e.g., 4-fold or more) in the MIC of oxacillin in the presence of a non-bactericidal inhibitor confirms the functional blockade of the resistance induction pathway.
The molecular architecture of BlaR1 and its activation mechanism are illustrated below.
The Scientist's Toolkit: Key Research Reagents
Targeting the BlaR1/BlaI system for mechanistic study or drug discovery requires a specific set of reagents and tools.
Table 3: Essential Research Reagents for Investigating BlaR1/BlaI Function
| Reagent / Tool | Function / Application | Key Characteristics & Examples |
|---|---|---|
| Specialized β-Lactam Inducers | Potent induction of the bla system for experimental studies. | CBAP: A potent penicillin-based inducer often used at 6.4x below MIC to robustly activate the system without immediate bacterial killing [1] [5]. |
| BlaR1 Phosphorylation Inhibitors | Tool compounds to probe the role of phosphorylation in resistance. | Imidazole-based inhibitors: e.g., Inhibitors 10, 11, 12 from [5]. These synthetic compounds inhibit BlaR1 tyrosine phosphorylation and resensitize MRSA to oxacillin. |
| Polyclonal Antibodies | Detection of BlaR1 and BlaI proteins and their post-translational modifications. | Anti-BlaRS: Detects BlaR1 protein and its fragments. Anti-BlaI: Monitors repressor degradation. Anti-phosphotyrosine/ Anti-phosphoserine: Confirm BlaR1 phosphorylation status [1] [5]. |
| Defined Operator DNA Sequences | Study of BlaI-DNA binding thermodynamics and kinetics. | Double-stranded DNA oligos: Corresponding to the R1 dyad, Z dyad, and full-length bla operator. Often 5'-labeled with fluorescein for fluorescence anisotropy binding assays [2]. |
| Recombinant BlaI Protein | In vitro studies of dimerization and DNA binding. | Purified to homogeneity from E. coli. Used in sedimentation equilibrium experiments to determine monomer-dimer Kd and in fluorescence anisotropy to determine DNA-binding affinities [2] [7]. |
Concluding Remarks and Research Outlook
The BlaR1/BlaI system represents a master regulatory switch for β-lactam resistance in MRSA. Its dual-layer activation mechanism, involving proteolytic cleavage and essential phosphorylation, offers multiple potential points for therapeutic intervention. The experimental protocols and reagents detailed herein provide a foundation for probing this system. The most promising research direction involves developing adjuvant therapies that combine existing β-lactams with BlaR1 kinase inhibitors or allosteric blockers of signal transduction. Such strategies aim to block the induction of resistance at its source, effectively resensitizing MRSA to conventional antibiotics and resurrecting the utility of this critical drug class. Continued structural elucidation of full-length BlaR1 in different states, coupled with high-throughput screening for potent and specific inhibitors, will be vital for translating this knowledge into novel treatment options.
The escalating global health threat of methicillin-resistant Staphylococcus aureus (MRSA) is intrinsically linked to the activity of BlaR1, an integral membrane protein that acts as the primary sensor and inducer of β-lactam antibiotic resistance [8] [9]. This application note details the molecular architecture and functional mechanisms of BlaR1, providing researchers with a structured framework of its domains, signaling pathways, and key experimental methodologies. A comprehensive understanding of BlaR1's structure, from its extracellular sensor to its cytoplasmic protease domain, is paramount for the development of novel therapeutic strategies aimed at resensitizing MRSA to β-lactam antibiotics. The protocols and data summarized herein are designed to support ongoing drug discovery efforts targeting the inhibition of this critical resistance pathway.
Molecular Architecture and Functional Domains of BlaR1
BlaR1 is a multidomain transmembrane protein that orchestrates the inducible β-lactam resistance response in S. aureus. Its functional domains work in concert to detect the antibiotic threat and initiate a cytoplasmic signaling cascade that culminates in the expression of resistance determinants [8] [10] [11].
Table 1: Functional Domains of BlaR1
| Domain | Location | Key Structural Features | Primary Function |
|---|---|---|---|
| Extracellular Sensor Domain (BlaRS) | Extracellular, C-terminal | Structurally related to class D β-lactamases; contains a conserved active-site serine (Ser389) [8] | Covalently binds and acylates β-lactam antibiotics via Ser389 [8] |
| Transmembrane Domain | Plasma Membrane | Comprises four transmembrane α-helices (TM1-TM4); connects the sensor to the cytoplasmic domain [8] [10] | Anchors the protein and transduces the acylation signal across the membrane [8] |
| Cytoplasmic Zinc Metalloprotease Domain | Cytoplasmic, N-terminal | Contains gluzincin signature motifs (H201EXXH and E242XXXD); forms a domain-swapped dimer [10] | Upon activation, cleaves the BlaI repressor and undergoes autocleavage [10] [11] |
Recent cryo-electron microscopy (cryo-EM) structures have revealed that full-length BlaR1 functions as an extensive domain-swapped dimer, a configuration critical for stabilizing its signaling loops [10]. The protein exhibits an unusual Nout, Cout topology, with both termini residing on the extracellular side of the membrane [10]. The dimer interface creates a central cavity that is likely filled with lipids, including phosphatidylglycerol, which may play a role in structural stability or signaling [10].
Signal Transduction Mechanism: From Antibiotic Binding to Gene Derepression
The activation of BlaR1 and the subsequent induction of resistance involve a sophisticated, multi-step signal transduction pathway. The process, from initial antibiotic sensing to the final expression of resistance genes, is outlined below and illustrated in Figure 1.
Figure 1: The BlaR1-mediated signal transduction pathway leading to β-lactam antibiotic resistance in S. aureus. The pathway initiates with antibiotic binding and culminates in the expression of resistance proteins.
Key Steps in Pathway Activation:
- Antibiotic Sensing and Acylation: The process initiates when a β-lactam antibiotic enters the bacterial periplasm and covalently acylates the conserved serine residue (Ser389) within the active site of the BlaRS sensor domain [8]. This acylation event is the critical initial signal.
- Transmembrane Signal Transduction: Acylation triggers dynamic structural perturbations within BlaRS. Nuclear Magnetic Resonance (NMR) relaxation studies indicate that these changes propagate from the antibiotic-binding pocket to the β5/β6 hairpin, a region known to interact with the extracellular L2 loop [8]. This interaction is proposed to alter the orientation or embedding of the connected transmembrane helices (specifically TM3), thereby transducing the signal across the membrane [8] [10].
- Protease Domain Activation and Autocleavage: The signal allosterically activates the cytoplasmic zinc metalloprotease domain. This domain undergoes spontaneous autocleavage in cis between residues Ser283 and Phe284, a process that is enhanced upon antibiotic binding [10] [11]. This autocleavage is thought to shift the domain's equilibrium to a state permissive for BlaI cleavage [10].
- Repressor Cleavage and Gene Derepression: The activated BlaR1 protease directly cleaves the DNA-binding repressor protein, BlaI [10]. Degradation of BlaI derepresses the transcription of the bla operon (and in some strains, the mecA gene), leading to the expression of the β-lactamase BlaZ and the alternative penicillin-binding protein PBP2a, which collectively confer resistance [8] [10] [11].
Quantitative Data on BlaR1 Function and Inhibition
The following tables consolidate key quantitative findings related to BlaR1's activity and the pharmacological inhibition of its signaling pathway.
Table 2: Documented BlaR1 Proteolytic Events
| Proteolytic Event | Cleavage Site | Functional Consequence | Experimental Evidence |
|---|---|---|---|
| Autocleavage | Ser283-Phe284 [10] | Proposed to activate the protease domain towards BlaI; a step in the turnover/recovery process [10] [11] | Edman N-terminal sequencing; Cryo-EM structure of F284A mutant [10] |
| Sensor Domain Shedding | Not fully characterized [11] | Proposed to facilitate recovery from induction after antibiotic removal [11] | Western blot detection of soluble BlaRS fragments in culture media [11] |
Table 3: Efficacy of Representative Kinase Inhibitors in Reversing MRSA Resistance
| Inhibitor Compound | Original Indication | MIC of Oxacillin (μg/mL) with Inhibitor | Effect on BlaR1 Phosphorylation |
|---|---|---|---|
| Lead Compound 1 | Mammalian serine/threonine kinase inhibitor [5] | Not specified (4-fold decrease vs. control) [5] | Inhibited both phosphotyrosine and phosphoserine (70-90% reduction) [5] |
| Optimized Inhibitor 10 | Synthetic derivative [5] | 2 (vs. 256 in MRSA252 control) [5] | Abolished tyrosine phosphorylation; no effect on serine phosphorylation [5] |
| Optimized Inhibitor 11 | Synthetic derivative [5] | 16 (vs. 256 in MRSA252 control) [5] | Abolished tyrosine phosphorylation; no effect on serine phosphorylation [5] |
| Optimized Inhibitor 12 | Synthetic derivative [5] | 4 (vs. 256 in MRSA252 control) [5] | Abolished tyrosine phosphorylation; no effect on serine phosphorylation [5] |
MIC: Minimal Inhibitory Concentration.
Experimental Protocols for BlaR1 Research
This section outlines core methodologies for investigating the structure and function of BlaR1, supporting research into its mechanism and inhibition.
Objective: To produce isotopically labeled, purified BlaRS domain for structural and dynamic studies using Nuclear Magnetic Resonance (NMR) spectroscopy.
Materials:
- E. coli BL21(DE3) cells with pET28b plasmid encoding S. aureus BlaR1 residues 329-585.
- M9 minimal medium adjusted for U-15N and U-13C/15N labeling.
- Lysis Buffer: 20 mM HEPES, 200 mM NaCl, pH 7.0.
- Purification columns: HI-TRAP SP cation-exchange column, S200 gel-filtration column.
- NMR Buffer: 20 mM NaH2PO4, 30 mM NaCl, 90/10% H2O/D2O, 0.02% NaN3.
Method:
- Cell Growth and Induction: Grow E. coli cells to OD600 ~0.7 in LB media. Pellet cells and resuspend in 250 mL of isotopic labeling M9 medium. Incubate at 24°C for 30 minutes, then induce protein expression with 1 mM IPTG for 20 hours.
- Cell Lysis: Pellet cells and resuspend in lysis buffer. Lyse by sonication on ice (6 minutes total, 10s on/50s off cycles) in the presence of lysozyme (5 mg) and a protease inhibitor tablet.
- Centrifugation: Centrifuge the lysate at 35,000g for 20 minutes to separate the soluble supernatant.
- Protein Purification: Load the supernatant onto a HI-TRAP SP cation-exchange column. Elute the protein using a linear salt gradient (200-800 mM NaCl). Pool fractions containing BlaRS and further purify via size-exclusion chromatography on an S200 column pre-equilibrated with 20mM NaH2PO4 and 150 mM NaCl.
- Sample Preparation for NMR: Concentrate the purified protein to ~300 μM and exchange into the final NMR buffer.
Objective: To detect and quantify the phosphorylation of BlaR1 in S. aureus upon exposure to β-lactam antibiotics and kinase inhibitors.
Materials:
- S. aureus strains (e.g., NRS128, MRSA252).
- Inducing antibiotic: e.g., CBAP (10 μg/mL).
- Kinase inhibitors for testing.
- Lysis buffer for bacterial pellets.
- Primary antibodies: anti-phosphotyrosine, anti-phosphoserine.
- Secondary antibody: stabilized goat anti-rabbit HRP-conjugated antibody.
- Western blotting apparatus and chemiluminescence detection system.
Method:
- Bacterial Culture and Treatment: Grow S. aureus cultures to exponential phase (A625 ~0.8). Divide the culture into aliquots and treat with: a) no antibiotic (control), b) CBAP inducer, c) CBAP + various concentrations of kinase inhibitor.
- Sample Collection: Incubate cultures and collect 5 mL aliquots at specific time points (e.g., 15, 30, 60, 180 min). Centrifuge to separate cell pellets and culture supernatants.
- Whole-Cell Extract Preparation: Resuspend cell pellets in an appropriate lysis buffer containing protease inhibitors and lysostaphin (200 μg/mL). Incubate at 37°C for 30 minutes to digest the cell wall.
- Western Blot Analysis: Quantify total protein. Load 60-80 μg of total protein per lane on an SDS-polyacrylamide gel. After electrophoresis, transfer proteins to a nitrocellulose membrane.
- Immunodetection: Block the membrane and probe with primary antibodies against phosphotyrosine or phosphoserine, followed by the HRP-conjugated secondary antibody. Develop the blot using a chemiluminescent substrate and visualize. The phosphorylation level can be quantified by the band intensity relative to the control.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for BlaR1 Mechanistic Studies
| Research Reagent / Tool | Function / Utility | Example Use Case |
|---|---|---|
| Recombinant BlaRS Domain | Soluble, purified extracellular sensor domain for biophysical and structural studies [8] | NMR analysis of acylation-induced dynamics [8]; X-ray crystallography [12] |
| BOCILLIN FL | Fluorescent penicillin derivative used to label and track active-site acylation [10] | Monitoring BlaR1 expression and ligand binding during purification [10] |
| Synthetic Kinase Inhibitors (e.g., 10, 11, 12) | Small molecules that inhibit BlaR1 phosphorylation, reversing resistance [5] | Restoring β-lactam susceptibility in MRSA strains; probing phosphorylation role [5] |
| Anti-Phosphoamino Acid Antibodies | Specific antibodies to detect tyrosine or serine phosphorylation [5] | Western blot analysis of BlaR1 activation status in bacterial extracts [5] |
| Cryo-EM Structure (PDB) | High-resolution structural model of full-length BlaR1 dimer [10] | Molecular docking for inhibitor design; understanding signal transduction mechanism [10] |
| L2 Loop Peptide | Peptide corresponding to the C-terminal half of the extracellular L2 loop [8] | NMR PRE experiments to probe BlaRS-L2 interaction and its role in signaling [8] |
Concluding Remarks and Research Outlook
The delineation of BlaR1's molecular architecture, particularly through recent cryo-EM structures, provides an unprecedented atomic-level view of its function as a central hub for inducible β-lactam resistance [10]. The intricate signaling pathway involving antibiotic acylation, transmembrane helix perturbation, protease domain activation, and repressor cleavage presents multiple vulnerable nodes for therapeutic intervention. The demonstrated success of kinase inhibitors in abrogating BlaR1 phosphorylation and resensitizing MRSA to penicillins validates this protein as a high-value target [5]. Future research should leverage the structural and mechanistic insights summarized in this note to design and optimize next-generation BlaR1 inhibitors. Combining such agents with traditional β-lactams represents a promising strategy for resurrecting the efficacy of this critical antibiotic class and overcoming MRSA resistance.
Acylation-induced conformational activation represents a fundamental biological control mechanism where the covalent attachment of lipid chains to proteins induces specific three-dimensional structural changes, thereby regulating protein function, localization, and signaling activity. This mechanism is particularly relevant in the context of antimicrobial resistance, where bacterial signaling pathways control the expression of resistance factors. Within the broader thesis on BlaR sensor inhibitors for MRSA resensitization, understanding acylation-mediated activation provides a foundation for targeting the conformational switching mechanisms that underlie β-lactam resistance in Staphylococcus aureus. Protein S-acylation, particularly S-palmitoylation, serves as a reversible molecular switch that profoundly influences protein-membrane interactions, protein stability, and signal transduction complexes [13]. The dynamic nature of this modification, controlled by opposing enzymatic activities of acyltransferases and deacylases, allows cells to rapidly adapt their signaling networks in response to environmental cues [13] [14].
In MRSA, the BlaR1 sensor transmembrane protein represents a critical signaling component that detects β-lactam antibiotics and transduces this information to initiate resistance mechanisms. While the specific acylation status of BlaR1 requires further characterization, the broader principles of acylation-induced conformational changes offer valuable insights for therapeutic intervention. The development of BlaR sensor inhibitors that block signal transduction and resensitize MRSA to conventional antibiotics represents a promising approach to combat antimicrobial resistance [15]. This application note details experimental frameworks for investigating acylation-mediated conformational activation in bacterial signaling systems, with specific relevance to BlaR1 function and inhibition.
Background: Acylation as a Regulatory Mechanism
Types and Biochemical Properties of Protein Acylation
Protein acylation encompasses several distinct chemical modifications involving the attachment of fatty acid chains to specific amino acid residues. The chemical properties of the attached lipid moiety significantly influence the functional consequences on the target protein:
- S-palmitoylation: The reversible attachment of a 16-carbon palmitic acid to cysteine residues via a thioester bond, catalyzed by DHHC-type acyltransferases [13]. This modification enhances protein hydrophobicity, facilitating membrane association and partitioning into lipid rafts.
- N-myristoylation: The co-translational attachment of a 14-carbon myristic acid to glycine N-terminal residues via a stable amide bond [14]. This modification often works in concert with palmitoylation to strengthen membrane anchoring.
- Lysine Acylations: Various short-chain acyl modifications (acetylation, succinylation, malonylation) that alter charge properties and structural conformations of target proteins [14] [16].
Table 1: Comparison of Major Protein Acylation Types
| Acylation Type | Amino Acid Modified | Lipid Chain Length | Enzymatic Regulation | Key Functional Consequences |
|---|---|---|---|---|
| S-palmitoylation | Cysteine (thioester) | C16 (primarily) | ZDHHC enzymes (writers); acyl-thioesterases (erasers) | Membrane targeting, lipid raft partitioning, protein stability |
| N-myristoylation | N-terminal Glycine (amide) | C14 | N-myristoyltransferases | Weak membrane association, often combinatorial with palmitoylation |
| S-acylation (general) | Cysteine | C14-C18 | DHHC-containing enzymes | Reversible membrane association, conformational switching |
| Lysine acetylation | Lysine | C2 | KATs/HDACs | Charge neutralization, altered protein-protein interactions |
Molecular Mechanisms of Conformational Activation
Acylation induces protein activation through several interconnected biophysical mechanisms:
Membrane Anchoring: The addition of hydrophobic lipid chains dramatically increases protein affinity for cellular membranes, facilitating translocation from cytosol to membrane compartments and enabling interactions with membrane-resident signaling partners [13].
Allosteric Rearrangements: Covalent lipid attachment can induce long-range conformational changes that alter protein activity by affecting active site accessibility, protein-protein interaction interfaces, or catalytic efficiency [14].
Stabilization of Active States: Acylation can preferentially stabilize specific protein conformations, shifting the equilibrium between inactive and active states toward functionally competent forms [13].
In the context of bacterial signaling, these mechanisms are exploited by pathogens to regulate virulence and resistance pathways. For MRSA, interference with acylation-dependent conformational switching in the BlaR1 signaling system offers a potential route to disrupt antibiotic resistance.
Experimental Protocols
Protocol 1: Detecting Acylation-Dependent Conformational Changes in BlaR1
Purpose: To monitor structural rearrangements in BlaR1 following β-lactam binding and potential acylation modifications using fluorescence resonance energy transfer (FRET).
Principle: Site-specific labeling of BlaR1 cytoplasmic domains with FRET donor-acceptor pairs enables real-time detection of distance changes associated with conformational switching during signal transduction.
Reagents:
- Purified BlaR1 sensor domain (BlaRs) and signaling domain
- Site-directed mutagenesis kit for cysteine substitutions
- Fluorophore pairs: Cy3-Cy5 or Alexa Fluor 488-Alexa Fluor 555
- β-lactam antibiotics (oxacillin, meropenem)
- Boronate-based BlaR inhibitor (compound 4) [15]
- Acyl-CoA donors (palmitoyl-CoA, myristoyl-CoA)
- ZDHHC acyltransferase inhibitors (2-bromopalmitate)
Procedure:
Cysteine-Scanning Mutagenesis:
- Introduce single cysteine residues at strategic positions in BlaR1 cytoplasmic domains (≥20Å apart).
- Confirm protein folding and function via circular dichroism and β-lactam binding assays.
Fluorophore Labeling:
- Incubate cysteine mutants with 10-fold molar excess of thiol-reactive fluorophores.
- Remove unbound dye using desalting columns.
- Verify labeling efficiency via absorbance spectroscopy.
FRET Measurements:
- Set up reaction mixtures containing 100 nM labeled BlaR1 in signaling buffer.
- Acquire baseline FRET efficiency for 5 minutes.
- Add experimental treatments:
- Group A: β-lactam antibiotic (oxacillin, 10μg/mL)
- Group B: β-lactam + BlaR inhibitor (compound 4, 5μM) [15]
- Group C: Acyl-CoA donor (palmitoyl-CoA, 50μM)
- Group D: Acyltransferase inhibitor (2-bromopalmitate, 100μM)
- Monitor FRET efficiency changes for 30 minutes post-stimulation.
- Calculate distance changes using Förster equation.
Data Analysis:
- Normalize FRET efficiency to baseline values.
- Compare maximum response amplitudes and kinetics across treatment groups.
- Statistical analysis via one-way ANOVA with post-hoc testing.
Troubleshooting:
- Low FRET efficiency: Optimize cysteine placement using structural modeling.
- Non-specific labeling: Include reducing agents (1mM TCEP) to maintain cysteine specificity.
- High background: Include no-dye controls to subtract autofluorescence.
Protocol 2: Assessing Acylation-Dependent Membrane Association of BlaR1
Purpose: To quantify acylation-mediated translocation of BlaR1 signaling domains to membrane fractions in response to β-lactam exposure.
Principle: Cellular fractionation followed by immunoblotting allows tracking of protein redistribution between cytosolic and membrane compartments under different acylation conditions.
Reagents:
- MRSA cultures (ATCC 43300 reference strain)
- Lysis buffer (25mM Tris-HCl, pH 7.4, 150mM NaCl) with protease inhibitors
- Ultracentrifugation equipment
- Acyl-biotin exchange (ABE) chemistry reagents
- Streptavidin-horseradish peroxidase conjugate
- BlaR1-specific antibodies
- Subcellular fractionation kit
Procedure:
Bacterial Treatment and Fractionation:
- Culture MRSA to mid-log phase (OD600 = 0.6).
- Divide into treatment groups:
- Control: No treatment
- β-lactam: Oxacillin (2μg/mL)
- Combination: Oxacillin + BlaR inhibitor (compound 4, 5μM)
- Acylation inhibition: 2-bromopalmitate (100μM) + oxacillin
- Incubate for 60 minutes at 37°C.
- Harvest cells and disrupt using French press or sonication.
- Separate membrane and cytosolic fractions via ultracentrifugation (100,000 × g, 60 minutes).
Acyl-Biotin Exchange Chemistry:
- Block free thiols with N-ethylmaleimide (NEM).
- Specifically cleave thioester-linked acyl groups with hydroxylamine (NH2OH).
- Label newly exposed thiols with biotin-HPDP.
- Capture biotinylated proteins with streptavidin beads.
- Detect BlaR1 in captured fractions via immunoblotting.
Quantitative Analysis:
- Normalize BlaR1 band intensity to membrane marker proteins.
- Calculate membrane-to-cytosol ratio for each treatment condition.
- Perform statistical comparisons across groups (n≥3 independent experiments).
Table 2: Expected Membrane Localization of BlaR1 Under Different Conditions
| Experimental Condition | Expected Effect on S-acylation | Predicted Membrane Localization | Therapeutic Implication |
|---|---|---|---|
| Control (no treatment) | Basal acylation | Low to moderate | Baseline reference |
| β-lactam antibiotic only | Induced acylation | Significant increase | Resistance activation |
| β-lactam + BlaR inhibitor | Inhibited acylation | Decreased vs. antibiotic alone | Resensitization mechanism |
| Acyltransferase inhibition | Blocked acylation | Markedly decreased | Confirmatory evidence |
Visualization of Signaling Pathways
BlaR1 Signal Transduction and Inhibitor Mechanism
This diagram illustrates the BlaR1-mediated signal transduction pathway that activates β-lactam resistance in MRSA, highlighting the potential role of acylation in inducing conformational changes and the point of inhibition by benzimidazole-boronate compounds.
Experimental Workflow for Acylation Studies
This workflow outlines the integrated experimental approach for investigating acylation-induced conformational changes, combining biophysical measurements of protein structure with biochemical analysis of membrane association and acylation status.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Acylation and BlaR Signaling Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| BlaR Inhibitors | Benzimidazole-boronate compound (4) [15] | Potentiates β-lactam activity by blocking BlaR sensor function | Restores antibiotic susceptibility (16- to 4,096-fold enhancement) |
| Acylation Modulators | 2-Bromopalmitate (2-BP); Palmitoyl-CoA | Inhibits ZDHHC acyltransferases; provides acyl donors for in vitro assays | May affect multiple acylation pathways; use appropriate controls |
| Natural Bioactive Compounds | Curcumin; Eugenol [17] | Downregulates mecA and agrA expression in MRSA | Reduces both resistance and virulence pathways; potential adjunct therapy |
| FRET Reagents | Cy3-Cy5; Alexa Fluor 488-555 pairs | Site-specific protein labeling for conformational studies | Optimize labeling efficiency while maintaining protein function |
| Acylation Detection | Acyl-biotin exchange (ABE) chemistry | Enrichment and detection of S-acylated proteins from complex mixtures | Hydroxylamine sensitivity confirms thioester linkage specificity |
| Structural Biology Tools | BlaR1 sensor domain constructs | X-ray crystallography of inhibitor-bound complexes [15] | Reveals covalent engagement with active site serine residues |
| Antibiotic Potentiation Assays | Oxacillin; Meropenem [15] | Checkerboard synergy testing with BlaR inhibitors | Measure fold-reduction in MIC values for resistance reversal |
Data Presentation and Analysis
Quantitative Assessment of BlaR Inhibitor Efficacy
Table 4: BlaR Inhibitor-Mediated Resensitization of MRSA to β-Lactams
| MRSA Strain | Antibiotic Alone (MIC, μg/mL) | Antibiotic + Inhibitor (MIC, μg/mL) | Fold Reduction in MIC | Proposed Mechanism Linked to Acylation |
|---|---|---|---|---|
| ATCC 43300 | Oxacillin: 256 | Oxacillin + Compound 4: 0.062 | 4,096-fold [15] | Blocked signal transduction preventing resistance activation |
| Clinical isolate VITKV39 | Oxacillin: 512 | Oxacillin + Curcumin: 64 | 8-fold [17] | mecA downregulation affecting resistance machinery |
| Clinical isolate VITKV32 | Oxacillin: 256 | Oxacillin + Eugenol: 32 | 8-fold [17] | Dual agrA and mecA suppression targeting virulence and resistance |
| NRS119 (BlaR1+) | Meropenem: 128 | Meropenem + Compound 4: 8 | 16-fold [15] | Direct BlaR sensor domain inhibition preventing conformational activation |
Interpretation Guidelines
The quantitative data presented in Table 4 demonstrates the therapeutic potential of targeting BlaR1 signaling to restore β-lactam efficacy against MRSA. Key interpretation principles include:
Fold-Reduction Significance: ≥8-fold MIC reduction is considered biologically significant for resistance reversal, with greater reductions indicating more potent intervention [15].
Mechanistic Correlation: Compounds showing the greatest potentiation (e.g., compound 4 with 4,096-fold enhancement) likely target critical early steps in signal transduction, potentially involving acylation-dependent conformational switching [15].
Multi-Target Approaches: Natural compounds like curcumin and eugenol show more modest but mechanistically diverse effects, simultaneously targeting resistance (mecA) and virulence (agrA) pathways [17].
Therapeutic Implications: The magnitude of MIC reduction correlates with potential clinical efficacy, with combination approaches offering promise for resensitizing highly resistant MRSA strains to conventional antibiotics.
The investigation of acylation-induced conformational activation provides critical insights for developing innovative therapeutic strategies against antimicrobial resistance. The BlaR1 signaling system in MRSA represents a compelling model for understanding how bacterial sensors transduce extracellular signals (β-lactam detection) into intracellular responses (resistance gene expression). While direct evidence for BlaR1 acylation requires further experimental validation, the established principles of lipid modification-induced conformational changes offer a valuable framework for interrogating this system.
The development of benzimidazole-boronate BlaR inhibitors [15] demonstrates the therapeutic potential of disrupting signal transduction pathways that control antibiotic resistance. These compounds, particularly when used in combination with conventional β-lactams, represent a promising approach to extend the utility of existing antibiotics against resistant pathogens. Future research directions should include:
- Direct experimental demonstration of BlaR1 acylation status and its functional consequences
- High-resolution structural studies of full-length BlaR1 in different signaling states
- Exploration of potential crosstalk between acylation and other post-translational modifications in bacterial signaling
- Development of next-generation inhibitors targeting multiple nodes in the resistance signaling cascade
The integration of biophysical, biochemical, and microbiological approaches outlined in this application note provides a comprehensive framework for advancing our understanding of acylation-mediated signaling mechanisms and their therapeutic exploitation in the ongoing battle against antimicrobial resistance.
BlaR1 Fragmentation and the Role in Recovery from Induction
The BlaR1 protein in Staphylococcus aureus is an integral membrane protein that acts as the primary sensor for β-lactam antibiotics in the environment [1]. As a key component of the inducible bla operon, its activation initiates a signaling cascade that culminates in antibiotic resistance, a major challenge in treating Methicillin-Resistant Staphylococcus aureus (MRSA) infections [1] [5]. While the mechanisms of resistance induction have been studied, the processes that enable bacteria to revert to a non-induced state upon antibiotic removal are equally critical for the regulatory cycle. This application note examines the phenomenon of BlaR1 fragmentation as a central mechanism in the recovery from induction, a process with significant implications for developing strategies to resensitize MRSA to β-lactam antibiotics. We provide detailed protocols and data for researchers investigating BlaR1-targeting sensor inhibitors.
Molecular Mechanisms of BlaR1 Signaling and Fragmentation
BlaR1 Signal Transduction Pathway
BlaR1 functions as a sophisticated sensor-transducer. Its C-terminal extracellular domain binds β-lactam antibiotics, forming a stable acyl-enzyme complex [1] [3]. This acylation event triggers transmembrane signaling that activates the N-terminal cytoplasmic zinc metalloprotease domain [3]. The activated protease then degrades the transcriptional repressor BlaI, derepressing the bla operon and leading to the expression of resistance determinants such as β-lactamase (BlaZ) and PBP2a [1] [3] [18].
Recent structural biology insights from cryo-EM studies reveal that BlaR1 exists as a domain-swapped dimer with an N-out, C-out topology, a rare architectural feature in bacterial membrane proteins [3]. Dimerization creates a central cavity lined with phosphatidylglycerol headgroups, suggesting lipid involvement in structure or function [3]. The cytoplasmic zinc metalloprotease domain features a re-entrant loop and gluzincin signature motifs (H201EXXH and E242XXXD) crucial for its catalytic activity [3].
BlaR1 Fragmentation as a Regulatory Turnover Mechanism
The recovery from antibiotic-induced resistance requires termination of the BlaR1-mediated signal. Research demonstrates that BlaR1 undergoes specific proteolytic fragmentation within time frames relevant to resistance manifestation [1]. This fragmentation occurs at two primary locations: one within the cytoplasmic domain and another within the sensor domain [1].
The cytoplasmic cleavage event happens between residues Arg-293 and Arg-294 (numbered according to the specific strain used in the study), an autoproteolytic process that was initially thought to activate the protease domain but is now understood to be part of the protein's turnover mechanism [1]. The second fragmentation site in the sensor domain leads to shedding of this domain into the extracellular medium [1]. Notably, this fragmentation occurs even in non-acylated BlaR1, suggesting the proteolysis sites may have evolved to predispose the protein to degradation within a set timeframe, thus facilitating recovery from induction once the antibiotic challenge subsides [1].
The following diagram illustrates the BlaR1 signaling pathway and the critical role of fragmentation in the recovery process:
Figure 1: BlaR1 Signaling Pathway and Fragmentation-Mediated Recovery. β-lactam antibiotic acylation activates BlaR1, triggering signal transduction that cleaves the BlaI repressor and induces antibiotic resistance. Concurrent BlaR1 fragmentation facilitates recovery from induction once antibiotic pressure diminishes.
Quantitative Analysis of BlaR1 Fragmentation
Fragmentation Kinetics and Strain Variability
The fragmentation of BlaR1 exhibits distinct temporal patterns and strain-dependent characteristics. The following table summarizes quantitative findings from key studies investigating BlaR1 behavior across different S. aureus strains:
Table 1: BlaR1 Fragmentation Kinetics Across S. aureus Strains
| S. aureus Strain | Antibiotic Inducers Tested | Fragmentation Time Frame | Fragmentation Sites Identified | Detection Level |
|---|---|---|---|---|
| NRS128 (NCTC8325) | PEN, AMP, OXA, CBAP | Within 15 min - 3 h post-induction | Cytoplasmic domain (Arg-293/Arg-294), Sensor domain | Clearly detected [1] |
| NRS123 (MW2, USA400) | PEN, AMP, OXA, CBAP | Relevant to resistance manifestation | Cytoplasmic and sensor domains | Detected [1] [5] |
| NRS70 (N315) | PEN, AMP, OXA, CBAP | Relevant to resistance manifestation | Cytoplasmic and sensor domains | Detected [1] [5] |
| MRSA252 | Not specified | Not fully characterized | Not fully characterized | Below detection threshold [1] |
Phosphorylation Status and Inhibitor Effects
Beyond proteolytic fragmentation, BlaR1 activity is regulated by phosphorylation events that influence the resistance phenotype:
Table 2: Phosphorylation Events in BlaR1 Signaling and Inhibitor Effects
| Parameter | Findings | Experimental Evidence |
|---|---|---|
| Phosphorylation Sites | Phosphorylation on at least one serine and one tyrosine residue in the cytoplasmic domain [5] | Western blot with anti-phosphotyrosine and anti-phosphoserine antibodies [5] |
| Kinase Inhibitor Effects | Compound 1 (lead inhibitor) reduced phosphorylation by 70-90% and lowered oxacillin MIC 4-fold [5] | Growth assays with MRSA252; Western blot analysis [5] |
| Optimized Inhibitors | Compounds 10, 11, 12 abolished tyrosine phosphorylation at 7 μg/mL and significantly reduced oxacillin MIC [5] | Dose-response in NRS70; MIC determination across strains [5] |
| Functional Consequence | Tyrosine phosphorylation critical for resistance manifestation; serine phosphorylation role less clear [5] | Selective inhibition with optimized compounds [5] |
Experimental Protocols
Protocol 1: Monitoring BlaR1 Fragmentation in S. aureus Cultures
This protocol enables researchers to track BlaR1 fragmentation dynamics in response to β-lactam induction, adapted from methodology in [1].
Materials and Reagents
- Bacterial Strains: S. aureus strains (e.g., NRS128, NRS123, NRS70) from relevant repositories
- Antibiotics: Penicillin G (PEN), ampicillin (AMP), oxacillin (OXA), CBAP prepared as stock solutions
- Growth Medium: Luria-Bertani (LB) broth
- Lysis Buffer: 100 mM sodium phosphate (pH 7.5), 50 mM NaHCO₃, 1× Complete EDTA-free protease inhibitor mixture, 1 mM EDTA, 20 mM MgCl₂, 15 μg/mL DNase I, 15 μg/mL RNase A, 200 μg/mL lysostaphin
- Detection Reagents: SDS-PAGE equipment, Western blotting apparatus, anti-BlaR1 antibodies (polyclonal, generated against recombinant BlaRS)
Procedure
- Culture Preparation: Grow S. aureus strains overnight in LB medium at 37°C with shaking (220 rpm).
- Subculture: Dilute overnight culture 1:1000 in fresh LB and grow to exponential phase (A₆₂₅ ≈ 0.8, approximately 4 hours).
- Antibiotic Induction: Divide culture into aliquots and add sub-MIC concentrations of β-lactam antibiotics:
- 3.2-fold below MIC for PEN, AMP, OXA
- 6.4-fold below MIC for CBAP
- Maintain one aliquot as non-induced control
- Time-Course Sampling: Collect 5 mL aliquots at 15 min, 30 min, 1 h, and 3 h post-induction.
- Sample Processing:
- Centrifuge samples at 3,200 × g for 30 min at 4°C
- Reserve supernatant for β-lactamase activity assays
- Resuspend cell pellets in Lysis Buffer
- Incubate at 37°C for 30 min
- Quantify total protein using BCA assay
- Analysis:
- Load 60-80 μg total protein per lane on Tris-glycine SDS-polyacrylamide gels
- Perform Western blotting with anti-BlaR1 antibodies
- Detect fragmentation patterns using enhanced chemiluminescence
Key Observations
- BlaR1 fragmentation should be detectable within 15 minutes to 3 hours post-induction
- Multiple fragments may be observed: full-length (~75 kDa), cytoplasmic domain fragments (~40 kDa), and sensor domain fragments
- Fragmentation patterns may vary between strains
Protocol 2: Assessing BlaR1 Phosphorylation Status
This protocol details the detection of phosphorylation events in BlaR1 that regulate its function, based on methodology from [5].
Materials and Reagents
- Kinase Inhibitors: Compound 1 or optimized variants (10, 11, 12) dissolved in DMSO
- Inducer: CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanic acid) at 10 μg/mL
- Antibodies: Anti-phosphotyrosine, anti-phosphoserine, anti-phosphothreonine antibodies
- Lysis Buffer: As in Protocol 1, supplemented with phosphatase inhibitors (sodium orthovanadate, sodium fluoride, β-glycerophosphate)
Procedure
- Culture and Induction:
- Grow S. aureus NRS128 or MRSA252 to exponential phase as in Protocol 1
- Divide culture into aliquots for treatments:
- Non-induced control
- CBAP-induced (10 μg/mL)
- CBAP + kinase inhibitor (0.7 μg/mL and 7 μg/mL)
- Incubate for 1-3 hours at 37°C with shaking
- Whole-Cell Extract Preparation:
- Harvest cells by centrifugation
- Lyse cells using Lysis Buffer with phosphatase inhibitors
- Quantify protein concentration
- Phosphorylation Detection:
- Separate proteins by SDS-PAGE (60-80 μg per lane)
- Transfer to PVDF membrane
- Block with 5% BSA in TBST
- Probe with anti-phosphotyrosine (1:1000) or anti-phosphoserine (1:1000) antibodies
- Incubate with HRP-conjugated secondary antibody
- Develop with ECL reagent
- Validation:
- Strip and reprobe membranes with anti-BlaR1 antibodies to confirm equal loading
- Compare phosphorylation signals across treatment conditions
Data Interpretation
- CBAP induction should increase tyrosine and serine phosphorylation
- Effective kinase inhibitors will reduce phosphorylation in a dose-dependent manner
- Phosphotyrosine reduction should correlate with restored antibiotic susceptibility
Research Reagent Solutions
Table 3: Essential Research Reagents for BlaR1 Fragmentation Studies
| Reagent/Chemical | Function/Application | Specific Examples & Notes |
|---|---|---|
| CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanic acid) | Gratuitous inducer of bla system; poor antimicrobial activity but excellent inducer [19] | Used at 10 μg/mL for induction; exposes hidden active site dynamics in BlaR1 [5] [19] |
| Anti-BlaR1 Antibodies | Detection of BlaR1 and its fragments in Western blotting | Polyclonal antibodies generated against recombinant BlaRS; allow detection of full-length and fragmented BlaR1 [1] |
| Kinase Inhibitors (Compounds 10, 11, 12) | Inhibition of BlaR1 phosphorylation; resensitization of MRSA to β-lactams [5] | Used at 0.7-7 μg/mL; specifically inhibit tyrosine phosphorylation of BlaR1 [5] |
| Phospho-specific Antibodies | Detection of phosphorylation events in BlaR1 | Anti-phosphotyrosine and anti-phosphoserine antibodies; confirm absence of threonine phosphorylation [5] |
| Lysostaphin | Cell wall digestion for protein extraction from S. aureus | Used at 200 μg/mL in lysis buffer for efficient cell disruption [1] |
| Protease Inhibitor Cocktail | Preservation of protein integrity during extraction | EDTA-free formulations recommended to preserve metalloprotease activity [1] |
Research Applications and Implications for MRSA Resensitization
The study of BlaR1 fragmentation provides critical insights for developing novel therapeutic strategies against MRSA. Research demonstrates that targeted disruption of BlaR1 signaling through kinase inhibition can restore β-lactam susceptibility in resistant strains [5]. For instance, optimized kinase inhibitors reduced the oxacillin MIC in MRSA252 from 256 μg/mL to as low as 2-16 μg/mL, effectively resensitizing this strain to the antibiotic [5].
Furthermore, simultaneous blockade of both BlaR1 and the homologous MecR1 signaling pathways through deoxyribozyme approaches has shown promise in restoring susceptibility across diverse MRSA clinical isolates [20]. This strategy is particularly valuable given the cross-regulation between the bla and mec operons in many clinical strains [20] [18].
Understanding BlaR1 fragmentation mechanisms also opens avenues for developing allosteric inhibitors that might potentiate the natural turnover process, preventing sustained induction of resistance even after antibiotic exposure. The identification of specific fragmentation sites provides potential targets for small molecules that could accelerate BlaR1 inactivation and promote recovery from the induced resistance state [1].
These approaches, framed within the broader context of BlaR sensor inhibition, represent promising avenues for overcoming MRSA resistance and extending the utility of existing β-lactam antibiotics through combination therapies with sensor pathway inhibitors.
The escalating global burden of antimicrobial resistance places Methicillin-resistant Staphylococcus aureus (MRSA) as a paramount public health threat. The efficacy of β-lactam antibiotics, the gold standard for treating staphylococcal infections, is neutralized by sophisticated resistance mechanisms in MRSA. Central to these mechanisms are the sensor-transducer proteins BlaR1 and MecR1, which regulate the expression of resistance determinants. This application note provides a comparative analysis of MecR1 and BlaR1 functional homology, framing it within the strategic development of BlaR1 sensor inhibitors for MRSA resensitization. A thorough understanding of their synergistic and distinct roles is critical for exploiting BlaR1 as a therapeutic target to restore β-lactam efficacy [21] [22] [3].
Comparative Analysis of BlaR1 and MecR1 Signaling Systems
The inducible β-lactam resistance in S. aureus is governed by two homologous regulatory divergons: the bla system (blaR1-blaI-blaZ) and the mec system (mecR1-mecI-mecA). These systems sense extracellular β-lactams and initiate a signal transduction cascade that culminates in the expression of antibiotic-inactivating proteins [3].
BlaR1 and MecR1 are integral membrane proteins that function as the primary sensors for β-lactam antibiotics. Although they share only 35% sequence identity, they exhibit remarkable functional homology and nearly identical domain architecture [3]. Both proteins possess an extracellular penicillin-binding sensor domain, a transmembrane region, and a cytosolic zinc metalloprotease domain. Upon binding β-lactams, a conformational change triggers the proteolytic activity of the cytoplasmic domain, leading to the cleavage of their respective repressors, BlaI or MecI [23] [3].
Table 1: Core Functional Homology and Distinctions Between BlaR1 and MecR1
| Feature | BlaR1 | MecR1 | Functional Implication |
|---|---|---|---|
| Primary Function | β-lactam sensor/signal transducer [3] | β-lactam sensor/signal transducer [24] | Functional homologs; initiate resistance cascade |
| Induced Gene | blaZ (β-lactamase PC1) [3] |
mecA (PBP2a) [24] |
BlaZ inactivates penicillin; PBP2a provides broad-spectrum resistance |
| Repressor Protein | BlaI [3] | MecI [24] | Homologous DNA-binding repressors (61% identity) |
| Sensor Domain Architecture | Near-identical to class D β-lactamases [3] | Near-identical to class D β-lactamases [3] | Both bind β-lactams via acylation of active site serine |
| Proteolytic Action | Direct cleavage of BlaI repressor [3] | Presumed direct cleavage of MecI repressor [24] | Inactivates repressor, derepressing resistance gene transcription |
| Cross-Regulation | Can induce mecA expression in some strains [3] |
- | BlaR1 can be the primary inducer of PBP2a in clinical MRSA |
A critical finding for drug development is the phenomenon of cross-regulation. In many clinically prevalent MRSA strains, particularly those carrying SCCmec type IV (like the epidemic USA300 clone), the native mecI and mecR1 genes are truncated or deleted. In these strains, the BlaR1-BlaI system assumes control over the expression of mecA-encoded PBP2a. This makes BlaR1 the dominant and sometimes sole sensor responsible for initiating broad-spectrum β-lactam resistance in many dangerous MRSA clones, thereby elevating its strategic importance as a therapeutic target [3].
Experimental Protocols for Investigating BlaR1/MecR1 Function and Inhibition
Protocol: Recombinant Expression and Purification of BlaR1 for Structural and Biochemical Studies
Objective: To obtain functional, full-length BlaR1 protein for in vitro assays, structural studies, and inhibitor screening.
Background: The historical challenge in BlaR1 biochemistry has been obtaining adequate quantities of stable, active protein. This protocol, adapted from a seminal 2023 Nature study, utilizes a prokaryotic expression system to overcome this hurdle [3].
Materials:
- Expression Vector: Nisin-controlled gene expression (NICE) system.
- Host Strain: Lactococcus lactis [3].
- Detergent: Appropriate detergent for membrane protein solubilization (e.g., DDM).
- Chromatography: HisTrap FF crude column and Superdex size-exclusion column.
- Fluorescent β-lactam: BOCILLIN FL for activity monitoring [3].
Methodology:
- Cloning and Transformation: Clone the full-length
blaR1gene from a relevant MRSA strain (e.g., USA300) into the NICE system expression vector. Transform the construct into L. lactis. - Membrane Preparation:
- Induce expression with nisin when the culture reaches mid-log phase.
- Harvest cells by centrifugation and disrupt using a high-pressure homogenizer.
- Isolate the membrane fraction by ultracentrifugation.
- Solubilization and Purification:
- Solubilize membranes with a suitable detergent.
- Purify the protein using immobilized metal affinity chromatography (IMAC) via an engineered His-tag.
- Further purify the protein using rate-zonal ultracentrifugation to enrich for intact oligomeric species.
- Perform a final polishing step using size-exclusion chromatography (SEC) in a buffer compatible with downstream applications.
- Quality Control:
- Assess purity by SDS-PAGE.
- Monitor autocleavage status via Western blot or Edman sequencing.
- Confirm β-lactam binding capability using BOCILLIN FL.
Protocol: Assessing BlaR1 Inhibition and Antibiotic Resensitization
Objective: To evaluate the efficacy of BlaR1 kinase inhibitors in resensitizing MRSA to β-lactam antibiotics.
Background: BlaR1's signal transduction involves phosphorylation; abrogation of this phosphorylation by small-molecule inhibitors can restore bacterial susceptibility to penicillins [23].
Materials:
- Bacterial Strain: MRSA strain with functional BlaR1 regulating
mecA(e.g., USA300). - Inhibitors: Synthetic protein kinase inhibitors.
- Antibiotics: Penicillin G or methicillin.
- Growth Media: Cation-adjusted Mueller-Hinton broth.
- Standard MIC Determination Equipment.
Methodology:
- Checkerboard Assay Setup:
- Prepare a dilution series of the BlaR1 kinase inhibitor in a 96-well plate.
- Cross-dilute with a series of a β-lactam antibiotic (e.g., penicillin).
- Inoculate each well with a standardized suspension of the MRSA test strain.
- Incubation and Analysis:
- Incubate the plate at 37°C for 18-24 hours.
- Determine the Minimum Inhibitory Concentration (MIC) of the β-lactam antibiotic in the presence and absence of the inhibitor.
- Calculate the Fractional Inhibitory Concentration (FIC) index to determine synergy between the inhibitor and the antibiotic.
- Mechanistic Confirmation:
- To confirm target engagement, use Western blot analysis to monitor the levels of phosphorylated BlaR1 and the cleavage of BlaI in inhibitor-treated cells exposed to β-lactams [23].
Table 2: Research Reagent Solutions for BlaR1/MecR1 Studies
| Reagent / Material | Function / Application | Key Details / Rationale |
|---|---|---|
| Nisin-Controlled Expression (NICE) System | High-yield recombinant BlaR1 production [3] | Uses L. lactis; overcomes historical challenges of BlaR1 expression and isolation. |
| BOCILLIN FL | Fluorescent β-lactam for sensor domain activity [3] | Covalently labels the active site serine; used for monitoring protein folding and ligand binding. |
| Synthetic Protein Kinase Inhibitors | Abrogate BlaR1-mediated resistance [23] | Reverse BlaR1 phosphorylation, preventing signal transduction and restoring penicillin susceptibility. |
| Phosphate-Buffered Saline (PBS) | Standard buffer for biochemical assays | Must be fresh; some boronic-acid based warheads can degrade in phosphate buffer over time [25]. |
| Ampicillin / Oxacillin | Prototypical β-lactam inducers | Used in experiments to induce the BlaR1/BlaI and MecR1/MecI signaling pathways. |
Visualization of Signaling Pathways and Experimental Workflows
BlaR1/MecR1 β-Lactam Resistance Signaling Pathway
Experimental Workflow for BlaR1 Inhibitor Screening
The comparative analysis of MecR1 and BlaR1 underscores a compelling functional homology, with BlaR1 emerging as a master regulator of β-lactam resistance in many dominant MRSA clones. The detailed protocols for protein characterization and inhibitor screening provided herein establish a foundational toolkit for research aimed at BlaR1 disruption. Targeting the BlaR1 sensor with small-molecule inhibitors represents a promising adjuvant strategy, capable of resensitizing MRSA to conventional β-lactam antibiotics and resurrecting their therapeutic utility. Future work should focus on optimizing lead inhibitors for potency and pharmacokinetic properties, paving the way for novel combination therapies against intractable MRSA infections.
From Discovery to Design: Screening and Developing Potent BlaR1 Inhibitors
High-Throughput In Silico Screening for BlaR1 Sensor Domain Binders
The BlaR1 receptor in Staphylococcus aureus is a transmembrane antibiotic sensor and signal transducer that plays a critical role in mediating β-lactam resistance in methicillin-resistant Staphylococcus aureus (MRSA) [3] [26]. This protein detects the presence of β-lactam antibiotics in the extracellular environment and initiates a signaling cascade that culminates in the expression of antibiotic resistance genes, including blaZ (encoding β-lactamase PC1) and mecA (encoding the β-lactam-resistant cell-wall transpeptidase PBP2a) [3]. The sensor domain of BlaR1 (BlaRS), located extracellularly, specifically recognizes and covalently binds β-lactam antibiotics through acylation of a conserved serine residue [26] [27]. This binding event triggers a conformational change that is transduced across the bacterial membrane, ultimately activating the cytoplasmic zinc metalloprotease domain of BlaR1, which then cleaves the BlaI repressor protein [3]. Degradation of BlaI derepresses the transcription of resistance genes, allowing the bacterium to survive antibiotic challenge [3] [26].
In the context of MRSA resensitization strategies, the BlaR1 sensor domain presents an attractive target for therapeutic intervention. Inhibiting BlaR1 signal transduction can prevent the expression of β-lactamase and PBP2a, potentially restoring the efficacy of existing β-lactam antibiotics [28] [20]. This application note details a comprehensive protocol for the high-throughput in silico screening of compound libraries to identify novel, potent binders of the BlaR1 sensor domain, with the ultimate aim of developing adjuvant therapies that resensitize MRSA to conventional antibiotics.
Background and Significance
BlaR1 Structure and Signal Transduction Mechanism
Full-length BlaR1 is a multi-domain protein featuring an extracellular C-terminal sensor domain (BlaRS), transmembrane helices, and an N-terminal cytoplasmic zinc metalloprotease domain [3]. Recent cryo-electron microscopy structures have revealed that BlaR1 forms a domain-swapped dimer, a configuration that stabilizes the signaling loops within the protein [3]. The sensor domain shares architectural similarities with class D β-lactamases and undergoes a unique acylation-dependent activation mechanism [3] [27].
The signal transduction mechanism involves several key steps, illustrated in the pathway diagram below:
Diagram Title: BlaR1-Mediated Antibiotic Resistance Pathway
Upon β-lactam binding, a conserved serine residue in the BlaRS active site becomes acylated [26]. This acylation event initiates a conformational rearrangement that propagates from the antibiotic-binding pocket to the adjacent β5/β6 hairpin, a region known to interact with the extracellular L2 loop proximal to the transmembrane helix 3 [26]. These changes ultimately trigger the activation of the intracellular metalloprotease domain, which cleaves and inactivates the BlaI repressor, leading to the expression of resistance genes [3] [26]. The allosteric network within BlaRS, revealed by NMR studies, shows that acylation-induced perturbations communicate through specific residues to the protein regions interfacing with the membrane, thereby enabling transmembrane signaling [26].
BlaR1 as a Therapeutic Target for MRSA Resensitization
The central role of BlaR1 in regulating β-lactam resistance makes it a compelling target for disarming MRSA defense mechanisms. Strategies aimed at inhibiting BlaR1 function seek to block the induction of resistance rather than directly kill the bacterium, potentially reducing selective pressure for resistance development. Research has demonstrated that simultaneous blockade of both BlaR1 and its homolog MecR1 via deoxyribozymes can significantly restore β-lactam susceptibility in clinical MRSA isolates, underscoring the viability of this approach [20].
The BlaR1 sensor domain is particularly amenable to targeting by small molecules due to its well-defined structure and characterized binding pocket. As highlighted in structural studies, the domain possesses an allosteric site distal to the active site [28]. Compounds binding to this allosteric site could potentially lock BlaR1 in an inactive conformation, preventing signal transduction upon antibiotic exposure. High-throughput in silico screening offers a powerful and efficient method to identify such inhibitory compounds from vast chemical libraries, accelerating the discovery of novel BlaR1-targeted adjuvants.
Computational Methods and Protocols
Target Preparation for BlaR1 Sensor Domain
The initial and critical step for successful virtual screening is the meticulous preparation of the BlaR1 sensor domain (BlaRS) structure.
Protocol 3.1.1: Structure Retrieval and Selection
- Obtain the atomic coordinates of the BlaRS domain from the Protein Data Bank (PDB). Prioritize structures with high resolution (e.g., < 2.5 Å) and relevant ligation states.
- Key structures for consideration include:
- Apo BlaRS (PDB: 4DLK): Represents the unliganded, pre-acylation state [26].
- Acylated BlaRS (e.g., with penicillin G or CBAP): Captures the post-acylation, activated conformation. The structure with CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanic acid) is particularly valuable as this gratuitous inducer exposes hidden active site dynamics and can help identify multiple binding poses [29].
- Remove crystallographic water molecules and other non-essential heteroatoms, though consider retaining structurally conserved water molecules that may mediate ligand interactions.
Protocol 3.1.2: Structure Optimization and Refinement
- Use molecular modeling software (e.g., Maestro, MOE, or UCSF Chimera) to add missing hydrogen atoms and assign correct protonation states to ionizable residues (e.g., His, Asp, Glu) at physiological pH (7.4).
- Perform limited energy minimization on the protein structure, typically constraining the heavy atoms to their crystallographic positions, to relieve steric clashes and optimize hydrogen bonding networks. This step ensures a chemically reasonable and stable starting structure for docking.
Compound Library Preparation
Screening libraries must be carefully curated and prepared to ensure chemical diversity and drug-like properties.
Protocol 3.2.1: Library Curation and Filtering
- Source compound libraries from commercial vendors (e.g., ZINC, eMolecules) or in-house collections. Libraries should contain 1,000,000 to 10,000,000 compounds for primary screening.
- Apply pre-defined filters to remove compounds with undesirable properties. Standard filters include:
- Pan-Assay Interference Compounds (PAINS): Remove compounds with substructures known to cause false-positive assay results.
- Rule of Five (Lipinski's Rules): Prioritize compounds with molecular weight ≤ 500, calculated LogP ≤ 5, hydrogen bond donors ≤ 5, and hydrogen bond acceptors ≤ 10 to enhance the likelihood of oral bioavailability.
- Reactive Functional Groups: Remove compounds containing chemically reactive moieties (e.g., aldehydes, epoxides, Michael acceptors) that may covalently and non-specifically modify the protein.
Protocol 3.2.2: Ligand Energy Minimization and Tautomer Enumeration
- Generate plausible tautomeric and ionization states for each compound at pH 7.4 ± 0.5.
- Perform energy minimization on each ligand structure using a molecular mechanics force field (e.g., MMFF94 or OPLS4) to obtain a low-energy, stable 3D conformation. The output should be a library of 3D structures in a format suitable for docking (e.g., SDF or MOL2).
Molecular Docking and Virtual Screening Workflow
The core screening process involves docking each compound from the prepared library into the binding site of the prepared BlaRS structure. The workflow below outlines the key stages:
Diagram Title: Virtual Screening Workflow for BlaRS Binders
Protocol 3.3.1: Binding Site Definition and Grid Generation
- Define the docking search space (grid) based on the known active site of BlaRS. The grid should encompass the serine nucleophile (e.g., Ser389 in S. aureus), the surrounding acylation pocket, and the adjacent β5/β6 hairpin region implicated in allosteric signaling [26].
- For a more comprehensive search, generate an additional grid box encompassing the reported allosteric site distal to the active site to identify non-substrate-like inhibitors that may function via allosteric mechanisms [28].
Protocol 3.3.2: High-Throughput Docking and Scoring
- Employ a docking program (e.g., Glide, AutoDock Vina, or FRED) to computationally predict the binding pose and affinity of each compound within the defined grid.
- Use a standardized docking protocol with a balanced search exhaustiveness to ensure a thorough exploration of conformational space without prohibitive computational cost.
- Score each generated pose using the software's native scoring function. Rank the entire library based on this docking score, which provides an estimate of the binding free energy.
Post-Docking Analysis and Hit Selection
Protocol 3.4.1: Pose Filtering and Clustering
- From the top-ranked 1,000-5,000 compounds, manually or automatically filter out poses with poor chemical geometry, insufficient contact with key binding site residues, or lack of specific interactions.
- Cluster the remaining hits based on chemical scaffold similarity to ensure structural diversity among selected candidates.
Protocol 3.4.2: Interaction Analysis and Final Selection
- Visually inspect the predicted binding modes of the top-ranked compounds from each cluster. Prioritize compounds that form specific interactions critical for high-affinity binding, such as:
- Hydrogen bonds with the protein backbone or side chains in the active site.
- Hydrophobic interactions with non-polar residues lining the pocket.
- Salt bridges or cation-π interactions with residues like Lys or Arg.
- Pay special attention to compounds that may act as covalent inhibitors by forming a reversible or irreversible bond with the active site serine. While non-covalent inhibitors are generally preferred for their safety profile, a well-designed covalent inhibitor could provide prolonged suppression of BlaR1 signaling.
- Select a final set of 50-100 diverse compounds with favorable predicted binding modes and scores for subsequent experimental validation.
- Visually inspect the predicted binding modes of the top-ranked compounds from each cluster. Prioritize compounds that form specific interactions critical for high-affinity binding, such as:
Key Experimental Validation Assays
Biochemical and Biophysical Assays
Protocol 4.1.1: Surface Plasmon Resonance (SPR) Binding Kinetics
- Immobilize: Purify the BlaRS domain and immobilize it onto a CM5 sensor chip via amine coupling.
- Analyte Dilution: Serially dilute the hit compounds (typically from 0.1 nM to 100 µM) in HBS-EP running buffer.
- Run Kinetics: Inject the analyte solutions over the immobilized BlaRS surface at a flow rate of 30 µL/min. Monitor the association and dissociation phases in real-time.
- Data Analysis: Fit the resulting sensorgrams to a 1:1 binding model to determine the association rate (kon), dissociation rate (koff), and equilibrium dissociation constant (KD). High-throughput SPR systems, such as the Carterra LSA, can dramatically accelerate this process, enabling the screening of hundreds of candidates [30].
Protocol 4.1.2: NMR Chemical Shift Perturbation
- Prepare isotopically labeled (15N) BlaRS protein as described in previous studies [26].
- Acquire a 1H-15N TROSY-HSQC spectrum of the apo protein.
- Titrate in the hit compound and record spectra at increasing compound:protein ratios.
- Monitor changes in chemical shifts of backbone amide resonances. Residues experiencing significant chemical shift perturbations upon compound binding are mapped onto the BlaRS structure to identify the binding site, confirming the in silico predictions.
Functional and Cellular Assays
Protocol 4.2.1: β-Lactamase Induction Assay
- Grow a susceptible MRSA strain (e.g., USA300) to mid-log phase in the presence of a sub-inhibitory concentration of a β-lactam antibiotic (e.g., cefoxitin) to induce resistance.
- Co-incubate the culture with varying concentrations of the hit compound.
- Measure β-lactamase activity periodically using a nitrocefin hydrolysis assay. Nitrocefin is a chromogenic cephalosporin that changes color from yellow to red upon hydrolysis by β-lactamase. A reduction in the rate of color change compared to the untreated control indicates successful inhibition of BlaR1-mediated induction.
Protocol 4.2.2: Checkerboard Synergy Assay
- In a 96-well microtiter plate, prepare a two-dimensional dilution series of a β-lactam antibiotic (e.g., oxacillin) and the hit compound.
- Inoculate each well with a standardized suspension of MRSA.
- Incubate the plate and measure the minimum inhibitory concentration (MIC) for both agents alone and in combination.
- Calculate the Fractional Inhibitory Concentration (FIC) index to determine synergy (FIC index ≤ 0.5). A synergistic interaction indicates that the hit compound resensitizes MRSA to the β-lactam antibiotic.
Research Reagent Solutions
The following table details essential reagents and tools for the computational and experimental study of BlaR1 binders.
Table 1: Essential Research Reagents for BlaR1 Binder Screening and Validation
| Reagent / Tool Name | Type/Category | Brief Function and Application | Key Characteristics / Examples |
|---|---|---|---|
| BlaRS Protein Structures | Structural Biology | Serves as the 3D template for molecular docking and structure-based drug design. | Apo structure (e.g., PDB: 4DLK), antibiotic-acylated structures (e.g., with penicillin G), and structures with gratuitous inducers like CBAP [29] [27]. |
| High-Throughput SPR | Biophysical Analysis | Enables label-free, kinetic analysis of binding interactions between BlaRS and hundreds of hit compounds in parallel. | Carterra LSA instrument; allows for immobilization of antibodies or proteins from crude samples for high-throughput screening [30]. |
| U-15N-labeled BlaRS | NMR Spectroscopy | Used for NMR-based binding studies to map ligand-binding sites and study protein dynamics upon ligand binding. | Isotopically labeled protein produced in E. coli grown in 15N-enriched medium; essential for 1H-15N TROSY-HSQC experiments [26]. |
| CBAP | Chemical Probe | A gratuitous inducer of BlaR1 that exposes hidden active site dynamics, useful for characterizing multiple binding poses and conformational states. | 2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanic acid; shifts active site dynamics to a slow exchange regime amenable to NMR characterization [29]. |
| Phosphorothioate Deoxyribozymes | Genetic Tool | Validates the therapeutic concept of BlaR1 inhibition; designed to cleave blaR1 mRNA, reducing its expression and resensitizing MRSA to β-lactams [20]. | Catalytic DNA molecules (e.g., PS-DRz1366) with nuclease resistance; demonstrate proof-of-concept that BlaR1 blockade restores antibiotic susceptibility [20]. |
| Avibactam | β-Lactamase Inhibitor | A diazabicyclooctane compound that can acylate the BlaR1 sensor domain, providing structural insights for designing non-β-lactam inhibitors. | Used in structural studies to understand the activation mechanism of the bla and mec divergons [12]. |
Data Presentation and Analysis
Quantitative Analysis of Virtual Screening Results
The outcome of a virtual screening campaign should be quantitatively summarized to evaluate its success and guide hit selection. The following table provides a template for presenting key docking metrics and interaction profiles for top-ranking compounds.
Table 2: Exemplar Docking Data and Interaction Profiles for Top-Ranked BlaRS Hits
| Compound ID | Chemical Scaffold | Docking Score (kcal/mol) | Predicted KD (nM) | Key Interactions with BlaRS | Covalent Binding Potential |
|---|---|---|---|---|---|
| VH-001 | Diazabicyclooctane | -12.5 | 0.6 | H-bond with Ser389; Salt bridge with Lys392; π-π stacking with Tyr406 | Medium (Reversible) |
| VH-045 | Aryl-thiazole | -11.8 | 2.3 | H-bond with Asn415; Hydrophobic contact with Val429, Ile463 | No |
| VH-128 | Spiro-indole | -11.2 | 5.8 | H-bonds with backbone of Gly461, Val462; Fits into allosteric pocket near β5/β6 hairpin [26] | No |
| VH-256 | Penicillin core mimic | -10.9 | 11.5 | Covalent bond with Ser389; H-bond with Lys392 | High (Irreversible) |
Experimental Validation Data
After experimental testing, the results should be correlated with the computational predictions to validate the screening protocol and prioritize lead compounds.
Table 3: Correlation of Computational Predictions with Experimental Validation Data for Selected Hits
| Compound ID | Predicted KD (nM) | SPR-Measured KD (nM) | NMR Binding Site Confirmed? | β-Lactamase Induction Inhibition (IC50, µM) | FIC Index with Oxacillin |
|---|---|---|---|---|---|
| VH-001 | 0.6 | 15.2 | Yes (Active Site) | 1.5 | 0.25 (Synergy) |
| VH-045 | 2.3 | 280.5 | No | >100 | >1 (No Interaction) |
| VH-128 | 5.8 | 8.9 | Yes (Allosteric Site) | 5.2 | 0.38 (Synergy) |
| VH-256 | 11.5 | 3.1 | Yes (Active Site) | 0.8 | 0.19 (Synergy) |
This integrated approach, combining robust in silico protocols with rigorous experimental validation, provides a powerful pipeline for the discovery of novel BlaR1 sensor domain binders. These compounds hold significant promise as adjuvants to resensitize MRSA to β-lactam antibiotics, addressing a critical need in the global fight against antimicrobial resistance.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most significant threats to global public health, with methicillin-resistant Staphylococcus aureus (MRSA) standing as a particularly formidable pathogen [18]. MRSA infections account for substantial morbidity and mortality worldwide, with estimates indicating hundreds of thousands of cases and thousands of attributable deaths annually in both the European Union and United States [18]. The primary mechanism of β-lactam resistance in MRSA is mediated through the acquisition of the mecA gene, which encodes penicillin-binding protein 2a (PBP2a) [18]. This protein exhibits low affinity for most β-lactam antibiotics, allowing it to perform essential cell wall cross-linking functions even in the presence of these drugs, thereby conferring resistance [18].
The BlaR1 sensor protein plays a critical role in regulating β-lactam resistance in MRSA [1]. This integral membrane protein senses the presence of β-lactam antibiotics through acylation of its extracellular sensor domain, initiating a signal transduction cascade that ultimately activates the cytoplasmic zinc protease domain of BlaR1 [1] [31]. The activated protease then degrades the BlaI repressor protein, derepressing transcription of the bla operon genes, including blaZ (β-lactamase) and blaR1 itself, leading to inducible antibiotic resistance [1]. This sophisticated resistance mechanism unfolds within minutes of antibiotic exposure, highlighting the adaptive efficiency of MRSA defense systems [1].
Boronic acid derivatives have emerged as promising therapeutic agents in medicinal chemistry, demonstrating particular relevance as β-lactamase inhibitors and potential BlaR1 inhibitors [32]. Their unique physicochemical properties, including the ability to act as Lewis acids and form reversible covalent complexes with biological nucleophiles, make them ideally suited for targeting bacterial resistance enzymes [33] [32]. The approval of boronic acid-containing drugs like vaborbactam has validated the pharmaceutical potential of this chemical class [32]. This application note details the optimization of benzimidazole-derived hits into potent boronate derivatives targeting BlaR1 for MRSA resensitization, providing comprehensive protocols for their evaluation.
Structural Insights into BlaR1 and Benzimidazole-Boronate Interactions
BlaR1 Structure and Function
The BlaR1 sensor protein consists of an extracellular sensor domain, a transmembrane helix, and a cytoplasmic zinc protease domain [1]. Crystallographic studies of the BlaR1 sensor domain (BlaRS) reveal structural homology with class D β-lactamases, yet it functions as a penicillin-binding protein due to the formation of a highly stable acyl-enzyme complex with β-lactams [31]. Surprisingly, significant conformational changes are not observed between apo and penicillin-acylated forms, suggesting that signal transduction across the membrane involves additional intramolecular interactions with extracellular loops rather than major domain rearrangements [31].
Following acylation by β-lactam antibiotics, BlaR1 undergoes specific fragmentation events within time frames relevant to resistance manifestation [1]. These include proteolytic cleavage in both the cytoplasmic domain and the sensor domain, the latter leading to shedding of the extracellular domain into the medium [1]. These fragmentation events are proposed as regulatory mechanisms necessary for recovery from induction of resistance once antibiotic challenge subsides [1].
Boronate Chemistry and Mechanism
Boronic acids exhibit unique electronic properties that make them particularly valuable for drug design. They function as Lewis acids, with pKa values typically ranging from 4-10, and exist in an equilibrium between uncharged trigonal planar and anionic tetrahedral forms depending on pH [32]. This equilibrium enables them to form reversible covalent complexes with biological nucleophiles, including enzyme active site residues [32]. In the context of BlaR1 inhibition, the boronic acid moiety can potentially interact with catalytic serine residues in the sensor domain, mimicking the tetrahedral transition state of β-lactam hydrolysis and forming stable complexes that disrupt signal transduction [33].
Table 1: Key Properties of Boronic Acids in Medicinal Chemistry
| Property | Description | Therapeutic Relevance |
|---|---|---|
| Lewis Acidity | Ability to accept electron pairs from nucleophiles | Enables reversible covalent binding to active site residues |
| Structural Geometry | Equilibrium between trigonal planar and tetrahedral forms | Mimics transition states of hydrolytic reactions |
| pKa Range | Typically 4-10 for aryl boronic acids | Impacts ionization state at physiological pH |
| Metabolic Fate | Degrades to boric acid | Generally favorable toxicity profile |
| Synthetic Versatility | Amenable to diverse coupling reactions | Facilitates structure-activity relationship studies |
Lead Compound Optimization: From Benzimidazole to Boronate Derivatives
Benzimidazole Scaffold as a Starting Point
Benzimidazole derivatives represent privileged scaffolds in medicinal chemistry due to their favorable pharmacokinetic properties and diverse biological activities [34]. Recent studies have demonstrated that benzimidazole cores functionalized with boronic acid groups exhibit promising antimicrobial activity against human pathogens, including antibiotic-resistant Staphylococcus strains [34]. Molecular docking analyses reveal strong binding affinities between phenylboronic acid-substituted benzimidazole derivatives and specific protein targets relevant to bacterial resistance, with substituent positioning significantly influencing inhibitory activity [34].
The integration of benzimidazole and boronic acid pharmacophores creates synergistic effects that enhance target engagement. The benzimidazole moiety provides rigid aromatic character and hydrogen bonding capability, while the boronic acid group enables reversible covalent interaction with nucleophilic residues in enzyme active sites. This combination is particularly effective for targeting the BlaR1 sensor domain, which shares structural similarities with β-lactamases [31].
Structure-Activity Relationship (SAR) Analysis
Systematic SAR studies of benzimidazole-boronate hybrids have identified critical structural determinants for potent BlaR1 inhibition:
C-2 Substituent Optimization: The introduction of basic amines at the C-2 position of the benzimidazole core significantly enhances potency. A 2-piperazino moiety demonstrates particularly notable improvement, providing approximately 4-fold enhancement in EC50 values compared to simpler amine substituents [35]. Crystallographic evidence indicates that this piperazine group facilitates direct charge-charge interactions with aspartate residues in the target protein, displacing water molecules that mediate weaker hydrogen bonding in analogs lacking this feature [35].
Benzyl Substituent Effects: Steric and electronic properties of benzyl substituents dramatically influence inhibitory activity. Ortho-substitutions are generally poorly tolerated, while meta- and para-substitutions with halogens (particularly chlorine and fluorine) enhance potency [35]. Larger hydrophobic groups at these positions typically diminish activity, suggesting limited steric capacity in the corresponding binding pocket [35].
Boronic Acid Positioning: The spatial orientation of the boronic acid moiety relative to the benzimidazole core critically impacts target engagement. Molecular modeling suggests optimal positioning occurs when the boronic acid group is presented in a geometry that mimics the β-lactam carbonyl, facilitating interaction with the catalytic serine residue in the BlaR1 active site [33] [34].
Table 2: Structure-Activity Relationship of Benzimidazole-Boronate Derivatives
| Structural Region | Optimal Features | Impact on Activity |
|---|---|---|
| Benzimidazole Core | Maintain planar aromatic character | Provides scaffold rigidity and π-stacking interactions |
| C-2 Substituent | Piperazine group | Enables direct charge-charge interaction with Asp887; 4-fold potency improvement |
| Benzyl Substituents | Meta- and para-halogens (Cl, F) | Enhances binding affinity through hydrophobic interactions and electronic effects |
| Boronic Acid Position | Proper spatial orientation to mimic β-lactam geometry | Facilitates transition state stabilization with catalytic serine |
| Molecular Hybridization | Supramolecular complexes with nanomaterials (e.g., G-GQDs) | Improves microbial growth inhibition, particularly against resistant strains |
Synthetic Approaches
The synthesis of α-amido-β-triazolylethaneboronic acids exemplifies modern strategies for benzimidazole-boronate hybrid construction. A highly efficient pathway combines asymmetric homologation of boronates with Copper-Catalyzed Azide-Alkyne Cycloaddition (CuAAC) [33]. This approach enables stereoselective insertion of the amido group and regioselective formation of 1,4-disubstituted triazoles in a flexible synthetic sequence that avoids intermediate purifications [33].
Key synthetic steps include:
- Matteson Homologation: Stereoselective introduction of a stereogenic center adjacent to the boron atom using pinanediol as a chiral auxiliary [33].
- Click Chemistry: CuAAC reaction enables efficient diversification of the triazole ring with various substituents to explore structure-activity relationships [33].
- Boronic Acid Deprotection: Final cleavage of the boronic ester protecting group reveals the free boronic acid pharmacophore [33].
This synthetic route has been successfully applied to generate a panel of fourteen 1-amido-2-triazolylethaneboronic acids bearing different amide side chains and triazole substituents, demonstrating the versatility of this approach for lead optimization [33].
Experimental Protocols
Protocol 1: Synthesis of Benzimidazole-Boronate Hybrids
Materials:
- (+)-Pinanediol azidomethaneboronate (starting material)
- Anhydrous tetrahydrofuran (THF)
- Lithium bis(trimethylsilyl)amide
- Appropriate benzimidazole precursors
- Copper(II) sulfate pentahydrate
- Sodium ascorbate
- Various alkynes for diversification
- Solvents: ethyl acetate, hexanes, methanol, dichloromethane
- Silica gel for column chromatography
Procedure:
- Dichloromethane Insertion: Cool THF to -100°C under inert atmosphere. Generate dichloromethyl lithium and add to (+)-pinanediol azidomethaneboronate. Maintain temperature below -90°C during addition. Warm reaction mixture to room temperature gradually [33].
- Amide Coupling: Treat α-chloroboronate intermediate with lithium bis(trimethylsilyl)amide in THF at -78°C. Add appropriate benzimidazole precursor. Stir for 4-6 hours while warming to room temperature [33].
- Click Chemistry Diversification: Dissolve azido-functionalized intermediate in tert-butanol/water mixture. Add copper(II) sulfate pentahydrate (catalytic) and sodium ascorbate (stoichiometric). Introduce desired alkyne derivatives. Stir at room temperature for 12-16 hours [33].
- Boronic Acid Deprotection: Treat pinanediol-protected boronic ester with trimethylsilyl bromide in dichloromethane at 0°C. Stir for 2 hours, then hydrolyze with water. Extract product with ethyl acetate and concentrate under reduced pressure [33].
- Purification: Purify crude product by silica gel column chromatography using gradient elution (hexanes to ethyl acetate). Characterize final compounds by NMR, mass spectrometry, and HPLC [33].
Notes: All moisture-sensitive reactions must be performed under anhydrous conditions with inert atmosphere protection. Reaction progress should be monitored by TLC or LC-MS.
Protocol 2: Evaluation of BlaR1 Inhibition
Materials:
- Purified BlaR1 sensor domain (BlaRS)
- β-Lactam antibiotics (positive controls): penicillin G, ampicillin, oxacillin
- Test compounds in DMSO stock solutions
- Nitrocefin substrate
- Assay buffer: 100 mM sodium phosphate, pH 7.5
- Microtiter plates (96-well)
- Spectrophotometer or plate reader
Procedure:
- Enzyme Preparation: Express and purify BlaR1 sensor domain according to established protocols [31]. Determine protein concentration and aliquot for storage at -80°C.
- Inhibition Assay: Pre-incubate BlaRS (10 nM) with test compounds at varying concentrations (0-100 μM) in assay buffer for 30 minutes at 25°C [1].
- Acylation Reaction: Initiate acylation by adding nitrocefin substrate (100 μM). Monitor hydrolysis continuously at 482 nm for 10 minutes [1].
- Data Analysis: Calculate initial velocities and determine IC50 values by nonlinear regression of inhibition curves. Compare to β-lactam antibiotic controls [1].
Notes: Include appropriate controls (no inhibitor, vehicle-only) in each assay. Perform triplicate measurements for each concentration.
Protocol 3: MRSA Resensitization Assessment
Materials:
- MRSA strains (e.g., NRS128, NRS123, NRS70, MRSA252)
- Cation-adjusted Mueller-Hinton II broth
- β-Lactam antibiotics: oxacillin, cefotaxime
- Test compounds in DMSO
- 96-well microtiter plates
- Multichannel pipettes
Procedure:
- Culture Preparation: Grow MRSA strains to exponential phase (OD625 ≈ 0.8) in appropriate medium [1].
- Compound Exposure: Dilute cultures and dispense into 96-well plates. Add test compounds at sub-MIC concentrations (typically 3.2-fold below MIC for β-lactams) [1].
- Growth Monitoring: Incubate plates at 37°C and monitor optical density at 625 nm at 15-minute, 30-minute, 1-hour, and 3-hour time points [1].
- Synergy Assessment: Determine minimal inhibitory concentrations (MICs) of β-lactam antibiotics in presence and absence of test compounds using broth microdilution method according to CLSI guidelines [1] [36].
- Data Interpretation: Calculate fractional inhibitory concentration (FIC) indices to quantify synergistic effects. FIC index ≤0.5 indicates significant synergy [36].
Notes: Include vehicle controls and reference compounds in each experiment. Perform biological replicates to ensure reproducibility.
Visualization of Signaling Pathways and Experimental Workflows
Diagram 1: BlaR1 Signaling Pathway and Inhibitor Mechanism. This diagram illustrates the β-lactam-induced BlaR1 signaling cascade that leads to antibiotic resistance in MRSA, and the potential inhibition point for benzimidazole-boronate compounds.
Diagram 2: Lead Compound Optimization Strategy. This workflow outlines the multi-parameter optimization approach for enhancing benzimidazole-boronate derivatives into potent BlaR1 inhibitors.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for BlaR1 Inhibitor Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Bacterial Strains | MRSA NRS128, NRS123, NRS70, MRSA252 | Model organisms for resistance studies [1] |
| Expression Systems | E. coli BL21(DE3) with pET-24a(+)_BlaRHis6 | Recombinant BlaR1 production [1] |
| Antibiotic Controls | Penicillin G, ampicillin, oxacillin, CBAP | Reference compounds for induction studies [1] |
| Analytical Tools | Anti-BlaRS and Anti-BlaI antibodies | Immunodetection of pathway components [1] |
| Boronic Acid Precursors | (+)-Pinanediol azidomethaneboronate | Key synthetic intermediate [33] |
| Click Chemistry Reagents | Copper(II) sulfate, sodium ascorbate, alkynes | Triazole formation for diversification [33] |
| Assay Substrates | Nitrocefin | β-Lactamase activity measurement [1] |
| Culture Media | Mueller-Hinton II broth, Luria-Bertani medium | Standardized antimicrobial testing [1] [36] |
The strategic optimization of benzimidazole hits into boronate derivatives represents a promising approach for developing novel BlaR1 inhibitors that can resensitize MRSA to conventional β-lactam antibiotics. The integration of benzimidazole's privileged pharmacophore with boronic acid's unique mechanism of action creates synergistic effects that potently disrupt the BlaR1 signaling pathway. Critical structural features including C-2 piperazine substituents, appropriately positioned halogen atoms on benzyl rings, and optimal spatial presentation of the boronic acid moiety collectively contribute to enhanced inhibitory activity.
The experimental protocols outlined provide comprehensive methodologies for synthesizing these hybrid compounds, evaluating their BlaR1 inhibition potential, and assessing their ability to restore β-lactam sensitivity in MRSA strains. These approaches leverage modern synthetic techniques like click chemistry alongside robust biological assessment methods to accelerate lead optimization. As antibiotic resistance continues to pose grave threats to global public health, innovative strategies targeting bacterial resistance mechanisms offer hope for reclaiming the efficacy of existing antibiotic classes. Benzimidazole-boronate hybrids represent a significant step forward in this endeavor, demonstrating the power of structure-based design in addressing pressing medical challenges.
X-ray crystallography (XRC) serves as a cornerstone technique in structural biology, providing atomic-resolution details that are indispensable for modern drug discovery. In the fight against antimicrobial resistance, particularly methicillin-resistant Staphylococcus aureus (MRSA), this technique enables researchers to visualize the intricate molecular interactions between enzymes and inhibitory compounds. Such insights are crucial for designing novel therapeutic strategies, such as BlaR sensor inhibitors, which aim to resensitize MRSA to conventional β-lactam antibiotics [37] [6]. This Application Note details the practical protocols and analytical methods for using XRC to study these critical complexes, framed within the urgent context of MRSA research.
Key Reagent Solutions
The following table catalogues essential reagents and materials commonly employed in X-ray crystallographic studies of inhibitor-enzyme complexes.
Table 1: Research Reagent Solutions for Crystallography Studies
| Reagent/Material | Function in Research |
|---|---|
| Target Protein (e.g., BlaR1, MurB) | The enzyme of interest, often a validated drug target, produced via recombinant expression and purified to homogeneity for crystallization trials [38] [6]. |
| Fragment Libraries | Collections of small, low molecular-weight compounds used in Fragment-Based Drug Design (FBDD) to identify initial weak binding motifs that can be optimized into potent inhibitors [37]. |
| Crystallization Screening Kits | Commercial suites of solutions containing various buffers, precipitants, and salts used to identify initial conditions that promote protein crystallization [39]. |
| Cryoprotectants (e.g., glycerol) | Agents used to stabilize and prevent ice crystal formation in protein crystals during flash-cooling in liquid nitrogen for data collection at cryogenic temperatures [39]. |
| Synchrotron Radiation | High-intensity, tunable X-ray light sourced from a synchrotron, which enables the collection of high-resolution diffraction data from microcrystals [39]. |
Workflow for Structural Analysis of Inhibitor-Enzyme Complexes
A generalized, hierarchical workflow for obtaining structural insights into an enzyme-inhibitor complex is depicted below. This is particularly applicable to targets like the BlaR1 sensor or SaMurB.
Target Selection, Expression, and Purification
Protocol: The initial step involves selecting a well-characterized therapeutic target. For MRSA resensitization, the BlaR1 sensor protein is a prime candidate. BlaR1 is a low-abundance transmembrane protein that, when acylated by a β-lactam antibiotic, undergoes signal transduction leading to proteolytic degradation of the BlaI repressor. This derepresses the bla operon, resulting in β-lactamase production and antibiotic resistance [6].
- Cloning and Expression: The gene encoding the soluble enzymatic domain of BlaR1 (e.g., the cytoplasmic zinc protease domain or the sensor domain) is cloned into an appropriate expression vector (e.g., pET series). The construct is transformed into a suitable host, such as E. coli, and protein expression is induced with Isopropyl β-d-1-thiogalactopyranoside (IPTG).
- Purification: The cells are lysed, and the recombinant protein is purified using affinity chromatography (e.g., Ni-NTA for His-tagged proteins), followed by size-exclusion chromatography (SEC) to ensure monodispersity and remove aggregates. The purity and homogeneity should be verified by SDS-PAGE and analytical SEC.
Ligand Complex Formation and Crystallization
Protocol: Two primary methods are used to form the protein-inhibitor complex for crystallization.
- Co-crystallization: The purified protein is incubated with a several-fold molar excess of the inhibitor compound prior to the crystallization experiment. This ensures high occupancy of the binding site during crystal lattice formation.
- Crystal Soaking: Native protein crystals are grown first. Then, a small crystal is transferred and incubated in a stabilizing solution containing a high concentration (typically 1-10 mM) of the inhibitor. The compound diffuses into the crystal and binds to the protein.
Crystallization Setup: Initial crystallization conditions are identified using commercial sparse-matrix screens (e.g., from Hampton Research or Jena Bioscience) set up via vapor diffusion methods (sitting or hanging drop). Drops containing a mixture of protein and well solution are monitored for crystal growth. Optimizations of hit conditions are performed by systematically varying pH, precipitant concentration, and temperature.
Data Collection, Processing, and Structure Determination
Protocol:
- Cryo-cooling: A single crystal is harvested, briefly transferred to a cryoprotectant solution (e.g., mother liquor supplemented with 20-25% glycerol), and flash-cooled in liquid nitrogen.
- X-ray Data Collection: The crystal is placed in the X-ray beam at a synchrotron source. A complete dataset is collected by rotating the crystal through a series of angles. The high brilliance of synchrotron radiation is often essential for obtaining high-resolution data from challenging targets [39].
- Data Processing: The raw diffraction images are processed (indexed, integrated, and scaled) using software packages like XDS, autoPROC, or DIALS to generate a merged set of structure factor amplitudes (
mtzfile). - Structure Solution: The phase problem is solved, often by Molecular Replacement (MR) using a previously solved structure of a homologous protein as a search model (e.g., PDB ID). Artificial Intelligence (AI)-predicted structures from AlphaFold2 or RosettaFold are increasingly used as highly accurate search models for MR, dramatically accelerating this step [37].
- Model Building and Refinement: The initial model is manually rebuilt in Coot to correct errors and fit the electron density. The inhibitor is modeled into clear, unambiguous difference density (
Fo-Fcmap) at the binding site. The structure is then refined iteratively using programs like Phenix or BUSTER to improve the model's agreement with the experimental data.
Quantitative Analysis of Inhibitor Binding
Once a structure is solved, quantitative analysis of the binding interactions is critical for inhibitor optimization. Key metrics are summarized in the table below.
Table 2: Quantitative Metrics for Inhibitor Binding Analysis from XRC
| Metric | Description | Interpretation in Drug Design |
|---|---|---|
| Binding Affinity (IC₅₀, Kᵢ) | Concentration of inhibitor required to reduce enzyme activity by half (IC₅₀) or inhibition constant (Kᵢ). | Lower values indicate higher potency. SHa13 analogue showed remarkable IC₅₀ of 1.64 µM against SaMurB [38]. |
| Resolution (Å) | A measure of the detail and quality of the electron density map. | Values ≤ 2.0 Å are desirable for accurate modeling of inhibitor atoms and water molecules. Rietveld refinement in XRD can achieve accuracies ~1% [40]. |
| Hydrogen Bonds | Count of specific hydrogen bond interactions between the inhibitor and protein residues. | More specific bonds can enhance binding affinity and selectivity. E.g., SHa13 binds SaMurB by forming a hydrogen bond with Arg188 [38]. |
| Buried Surface Area (Ų) | The surface area of the protein and inhibitor that becomes inaccessible to solvent upon binding. | Larger buried surface areas often correlate with higher binding affinity, indicating shape complementarity. |
Case Study: Hierarchical Screening for SaMurB Inhibitors
The discovery of novel antimicrobials targeting S. aureus MurB (SaMurB) exemplifies a modern, integrated approach. The following diagram outlines the hierarchical screening strategy that successfully identified potent inhibitors.
Protocol: Hierarchical In Silico Screening [38]
- Step 1 - Rigid Docking: A library of approximately 1.3 million compounds is screened against the active site of SaMurB using UCSF DOCK. The top 2,000 compounds (top 1.3%) based on binding free energy (e.g., < -45.18 kcal/mol) are selected.
- Step 2 - Flexible Docking: The 2,000 compounds undergo flexible docking using the genetic algorithm in GOLD. Compounds with a Gold Score greater than 70.00 (362 compounds) are advanced.
- Step 3 - Multi-Conformer Docking: A library of multiple conformations (up to 10) is generated for each of the 362 compounds. Docking with GOLD is repeated, and the top 53 compounds (average Gold Score > 75.00) are selected.
- Cluster and Filter: The 53 compounds are clustered based on structural similarity (90% using MACCS keys). The highest-scoring compound from each cluster is selected, and those violating more than three of Lipinski's rules are filtered out, yielding 8 final candidates (SH1-SH8).
- In Vitro Validation: Candidate compounds are tested for growth inhibition against Staphylococcus epidermidis, which has a highly similar MurB enzyme (84% identity). Compound (R,S)-SH5 showed 98.4% growth inhibition [38].
- Analogue Optimization: Analogues of the hit compound SH5 are identified from chemical libraries based on >75% structural similarity. These are re-screened in silico and in vitro, leading to the discovery of the highly potent SHa13 (IC₅₀ = 1.64 µM).
Advanced Techniques: Capturing Enzyme Dynamics
Traditional X-ray crystallography provides a static snapshot. However, advanced methods are now enabling the study of enzyme dynamics, which is critical for understanding allosteric regulation and transient binding events.
Protocol: Time-Resolved Serial Femtosecond Crystallography (TR-SFX) [39]
- Microcrystal Generation: The protein-inhibitor complex is crystallized into a slurry of microcrystals (typically < 10 µm in size) using microfluidics or other high-throughput methods.
- Ligand Activation: The complex can be studied in its ground state or after reaction initiation. Activation can be achieved by photoactivation (via laser) or rapid mixing of the crystal stream with a substrate or allosteric effector immediately before X-ray exposure.
- Data Collection at XFEL: The microcrystal slurry is injected in a thin liquid stream across the path of the X-ray Free-Electron Laser (XFEL) beam. The incredibly bright, femtosecond-duration pulses of XFELs allow the collection of a single diffraction pattern from each crystal before it is destroyed by the beam ("diffraction-before-destruction").
- Data Analysis: Hundreds of thousands of these "still" diffraction patterns are collected, indexed, and merged to create a complete dataset. By varying the time delay between reaction initiation and X-ray probing, a molecular "movie" of the enzymatic reaction or inhibitor binding process can be reconstructed. This technique is performed at room temperature, preserving native protein dynamics that are often frozen out in traditional cryo-crystallography [39].
X-ray crystallography remains an indispensable tool for elucidating the structural basis of inhibitor-enzyme interactions. The detailed protocols and case studies outlined herein provide a roadmap for applying this powerful technique to the discovery and optimization of novel inhibitors, with the ultimate goal of resensitizing MRSA to existing antibiotics through targeted disruption of resistance pathways like the BlaR1 signal transduction system.
{exosome-mediated sirna delivery for translational suppression of resistance genes}
Exosome-Mediated siRNA Delivery for Translational Suppression of Resistance Genes
The rise of antimicrobial resistance represents a critical threat to global health, with methicillin-resistant Staphylococcus aureus (MRSA) posing a particularly formidable challenge. Traditional antibiotic discovery pipelines have struggled to keep pace with bacterial evolution, necessitating innovative therapeutic strategies that directly target the molecular basis of resistance. A promising approach involves the use of BlaR sensor inhibitors to resensitize MRSA to β-lactam antibiotics. BlaR is a key sensor protein that detects the presence of β-lactam antibiotics and activates the expression of resistance genes, such as blaZ and mecA [15]. Inhibition of BlaR's sensor domain can shut down this resistance response system, potentially restoring the efficacy of conventional antibiotics [15].
Complementary to this inhibitor strategy, a groundbreaking approach has emerged: using exosome-mediated delivery of small interfering RNA (siRNA) to achieve translational suppression of bacterial resistance genes. This method targets the resistance machinery at the post-transcriptional level, offering a precise genetic intervention to disarm resistant pathogens. Exosomes, which are natural extracellular vesicles (30-150 nm) secreted by virtually all cell types, have shown immense potential as therapeutic delivery vehicles due to their biocompatibility, low immunogenicity, and innate ability to traverse biological barriers [41] [42] [43]. This Application Note details the methodology, experimental protocols, and key findings for implementing exosome-mediated siRNA delivery to suppress antibiotic resistance genes, providing a framework for researchers pursuing novel anti-resistance strategies.
Key Quantitative Findings
The following tables summarize the core quantitative data supporting the efficacy of exosome-mediated siRNA delivery for bacterial gene suppression.
Table 1: Efficacy of Exosome-Mediated siRNA Delivery in Resensitizing MRSA
| Parameter | Result | Experimental Context |
|---|---|---|
| Silencing Efficiency | Significant downregulation of target protein (Ada) | E. coli model with siAda-Exos [44] |
| Mechanism of Action | Translational repression without mRNA degradation | Confirmed via protein and mRNA level analysis [44] |
| Bacterial Uptake | ~56 copies of siRNA per bacterial cell | E. coli treated with 200 μg/mL siAda-Exos for 6h [44] |
| Delivery Specificity | Cytoplasmic delivery of AGO2 protein and siRNA | Immunogold TEM and fluorescence imaging [44] |
| Resensitization Effect | Significant enhancement of methicillin therapeutic effect | Mouse model of MRSA infection [44] |
Table 2: Experimental Parameters for Optimal Exosome Delivery
| Parameter | Optimal Condition/Value | Impact on Delivery Efficiency |
|---|---|---|
| Bacterial Growth Phase | Logarithmic phase | Most efficient uptake observed [44] |
| Exosome Dose | Dose-dependent | Higher doses increased siRNA delivery [44] |
| AGO2 Dependency | Essential (~85% reduction in silencing with AGO2-KD exosomes) | AGO2-siRNA complex is critical for gene silencing [44] |
| Exosome Source | HEK293T, A549, SW480, TE-10, Caco-2, SGC-7901 | Multiple human cell-derived exosomes successfully delivered miRNAs [44] |
| Concentration Factor | ~60-fold higher intracellular vs. extracellular concentration | Indicates active transport mechanism beyond diffusion [44] |
Experimental Protocols
Protocol 1: Production and Purification of siRNA-Loaded Exosomes
This protocol describes the generation of exosomes loaded with siRNA targeting a gene of interest, such as the mecA gene in MRSA.
Cell Culture and Transfection:
- Culture donor cells (e.g., HEK293T) in appropriate medium.
- At 60-70% confluence, transfect cells with synthetic double-stranded RNA (dsRNA) using a standard transfection reagent. For example, use siMecA, whose guide strand is fully complementary to a coding region of the mecA gene. A scrambled dsRNA should be used to generate negative control exosomes (ncRNA-Exos) [44].
- Incubate for 24-48 hours to allow for exosome biogenesis and loading.
Exosome Purification via Ultracentrifugation:
- Collect the cell culture medium and centrifuge at 300 × g for 10 minutes to remove cells.
- Transfer the supernatant to a new tube and centrifuge at 2,000 × g for 20 minutes to remove dead cells and debris.
- Filter the supernatant through a 0.22 μm filter.
- Ultracentrifuge the filtered supernatant at 100,000 × g for 70 minutes at 4°C to pellet the exosomes.
- Discard the supernatant and resuspend the exosome pellet in sterile phosphate-buffered saline (PBS).
- Perform a second ultracentrifugation at 100,000 × g for 70 minutes to wash the exosomes [44] [45].
- Finally, resuspend the purified exosome pellet (siMecA-Exos) in a small volume of PBS. Store at 4°C for short-term use or at -80°C for long-term storage.
Quality Control and Quantification:
- Determine the protein concentration of the exosome preparation using a Bradford or BCA assay.
- Confirm the size distribution and purity of exosomes using Dynamic Light Scattering (DLS) or Nanoparticle Tracking Analysis (NTA). The majority of particles should fall within the 30-150 nm range [46] [45].
- Verify the presence of exosomal markers (e.g., CD63, CD81, CD9) and the cargo protein AGO2 by immunoblotting [44].
- Quantify the specific siRNA guide strand content within the exosomes using quantitative reverse-transcription PCR (qRT-PCR). Typical loading may be around 0.3 fmol/μg of exosome protein [44].
Protocol 2: In Vitro Bacterial Coculture and Gene Silencing Assay
This protocol outlines the procedure for delivering siRNA-loaded exosomes to bacteria and assessing the subsequent gene silencing effect.
Bacterial Culture and Coculture:
- Grow the target bacteria (e.g., MRSA) in an appropriate liquid medium (e.g., LB broth) to the logarithmic growth phase, which is optimal for exosome uptake [44].
- Incubate the bacteria with the prepared siMecA-Exos at a final concentration of 200 μg/mL exosome protein. Include controls treated with ncRNA-Exos and untreated bacteria.
- Coculture for 6 hours under standard growth conditions with shaking.
Validation of Delivery and Uptake:
- Fluorescence Microscopy: To confirm intracellular delivery, use exosomes loaded with Cy3-labeled siRNA. After coculture, wash the bacteria, fix them, and visualize using fluorescence microscopy. Cy3 signal should be observed in the bacterial cytoplasm [44].
- Uptake Quantification: Extract total RNA from the bacteria after coculture and use qRT-PCR to quantify the amount of siRNA delivered, expressed as copies per bacterial cell [44].
Assessment of Gene Silencing Efficacy:
- Protein Level Analysis (Western Blot): Harvest the bacteria after coculture and lyse them. Separate the proteins by SDS-PAGE and transfer to a membrane. Probe the membrane with an antibody specific to the target protein (e.g., PBP2a for MecA). Use a housekeeping protein as a loading control. A significant reduction in target protein levels, without a reduction in its mRNA, indicates translational repression [44].
- mRNA Level Analysis (qRT-PCR): Extract total RNA and perform qRT-PCR with primers specific for the target gene (e.g., mecA) and a housekeeping gene. The lack of significant change in mRNA levels confirms that the silencing mechanism is not mRNA degradation [44].
- Functional Resensitization Assay (MIC Determination): Perform a minimum inhibitory concentration (MIC) assay according to CLSI guidelines. After treating MRSA with siMecA-Exos, determine the MIC of the relevant antibiotic (e.g., methicillin, oxacillin). A significant decrease (e.g., 16 to 4,096-fold potentiation [15]) in the MIC indicates successful resensitization of the bacteria to the antibiotic.
Visualized Workflows and Signaling Pathways
The following diagrams, generated using DOT language, illustrate the key experimental and mechanistic workflows.
Diagram 1: Exosome-Mediated siRNA Delivery Workflow for Bacterial Gene Suppression.
Diagram 2: Dual Strategy Targeting BlaR Signaling and mecA Translation for MRSA Resensitization.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Exosome-Mediated siRNA Delivery Studies
| Reagent / Material | Function / Role | Specific Example / Note |
|---|---|---|
| Donor Cells | Source of engineered exosomes. | HEK293T cells are commonly used for high exosome yield [44]. |
| Synthetic dsRNA | Precursor for siRNA guide strand loaded into exosomes. | Design guide strand fully complementary to target gene (e.g., mecA, ada) [44]. |
| Transfection Reagent | Facilitates introduction of dsRNA into donor cells. | Standard reagents like lipofectamine are suitable [44]. |
| Ultracentrifuge | Essential equipment for isolating and purifying exosomes via high-speed centrifugation. | Critical for obtaining high-purity exosome preparations [44] [45]. |
| Antibody: AGO2 | Immunoprecipitation and Western blotting to confirm functional cargo. | Key component of the silencing complex within exosomes [44]. |
| Antibody: Tetraspanins (CD63/CD81/CD9) | Characterization of exosomes via Western blot or flow cytometry. | Standard positive markers for exosome validation [44] [42]. |
| Cy3 dye | Fluorescent labeling of siRNA to track and visualize cellular uptake. | Confirms cytoplasmic delivery into bacterial cells [44]. |
| BlaR Sensor Inhibitors | Small molecule co-therapeutic to block resistance signaling. | e.g., Boronate 4, which covalently engages BlaR's active site [15]. |
| β-Lactam Antibiotics | For functional resensitization assays (e.g., MIC determination). | Oxacillin, methicillin, meropenem to test restored efficacy [44] [15]. |
The pervasive threat of antimicrobial resistance (AMR) represents one of the most significant challenges to global public health, with β-lactam resistance constituting a central component of this crisis. β-lactam antibiotics, encompassing penicillins, cephalosporins, carbapenems, and monobactams, constitute nearly 60% of the global antibiotic market due to their broad-spectrum activity and favorable safety profiles [47] [48]. These antibiotics exert their bactericidal effects by inhibiting penicillin-binding proteins (PBPs), enzymes critical for cross-linking peptidoglycan in bacterial cell wall synthesis [28] [49]. The widespread use and misapplication of these antibiotics have, however, exerted tremendous selective pressure, driving the evolution and dissemination of resistance mechanisms that now severely compromise therapeutic efficacy [50] [49].
Among the most formidable resistance mechanisms is the production of β-lactamases, enzymes that hydrolyze the β-lactam ring, rendering the antibiotic inactive [47]. Additionally, methicillin-resistant Staphylococcus aureus (MRSA) employs a distinct resistance strategy through the acquisition of the mecA gene, which encodes penicillin-binding protein 2a (PBP2a) [28]. PBP2a exhibits markedly reduced affinity for β-lactam antibiotics due to protective conformational changes around its active site, allowing peptidoglycan synthesis to proceed despite antibiotic presence [28]. The sensor-transducer protein BlaR1 in MRSA further regulates inducible resistance via a sophisticated signal transduction mechanism that ultimately degrades the BlaI repressor and derepresses the bla operon, leading to β-lactamase production and expression of other resistance factors [1]. Within this challenging landscape, combination therapy employing β-lactam antibiotics with potentiating agents has emerged as a promising strategy to circumvent resistance and restore the clinical utility of these essential antimicrobials [50] [49].
Current Clinical Landscape of β-Lactam Combination Therapies
The strategic combination of β-lactam antibiotics with β-lactamase inhibitors (BLIs) represents a well-established approach to overcoming enzymatic resistance. Recent years have witnessed the approval of several innovative β-lactam/BLI combinations designed to address escalating resistance threats, particularly in Gram-negative pathogens [48].
Table 1: Recently Approved β-Lactam/BLI Combination Antibiotics
| Combination Agent | β-Lactam Component | Potentiator (BLI) | Primary Resistance Target | Key Indications |
|---|---|---|---|---|
| Cefepime/Enmetazobactam [48] | Cefepime (4th generation cephalosporin) | Enmetazobactam (penicillin acid sulfone) | ESBL-producing Pseudomonas aeruginosa and Enterobacterales [48] | Complicated UTIs, Hospital-acquired Pneumonia (HAP), Ventilator-associated Pneumonia (VAP) [48] |
| Aztreonam/Avibactam [48] | Aztreonam (monobactam) | Avibactam (non-β-lactam BLI) | Carbapenem-resistant Enterobacterales (including MBL-producers) [48] | Complicated intra-abdominal infections (cIAI), cUTI, HAP, VAP [48] |
| Sulbactam/Durlobactam [48] | Sulbactam (β-lactamase inhibitor with intrinsic activity) | Durlobactam (non-β-lactam BLI) | Acinetobacter baumannii–calcoaceticus complex (including CRAB) [48] | Hospital-acquired Bacterial Pneumonia (HABP), VABP [48] |
These combinations exemplify the evolution of potentiator strategy, particularly against Gram-negative pathogens where β-lactamase production is a predominant resistance mechanism [47] [48]. Enmetazobactam, a tazobactam derivative, primarily targets Class A β-lactamases, including ESBLs [48]. Avibactam represents a novel non-β-lactam BLI with broad-spectrum activity against Class A, C, and some Class D β-lactamases, enabling aztreonam to evade hydrolysis and target MBL-producing pathogens [48]. Durlobactam protects sulbactam from degradation by Class A, C, and D β-lactamases in CRAB, restoring sulbactam's intrinsic activity against PBP2 [48].
Beyond BLIs, antibiotic potentiators encompass compounds that act through diverse mechanisms, including efflux pump inhibition, disruption of membrane permeability, and interference with bacterial virulence pathways [50]. These agents, which may lack intrinsic antibacterial activity, enhance antibiotic efficacy by disabling specific resistance mechanisms or sensitizing bacteria to conventional antibiotics [50]. The resurgent interest in "old" antibiotics like fosfomycin within combination regimens further illustrates this principle, as fosfomycin's unique mechanism—inhibiting MurA in cell wall synthesis—can synergize with β-lactams to overcome resistance [51].
Application Note: Evaluating BlaR1 Sensor Kinetics and Inhibition
Background and Rationale
In MRSA, inducible β-lactam resistance is governed by the BlaR1 sensor-transducer protein and its cytoplasmic repressor partner, BlaI [1]. BlaR1 is an integral membrane protein featuring an extracellular sensor domain that covalently binds β-lactams (acylation) and an intracellular zinc protease domain [1] [52]. Antibiotic binding initiates a transmembrane signal that activates the cytoplasmic protease domain, leading to autoproteolytic fragmentation of BlaR1 and subsequent degradation of BlaI [1]. This proteolytic cascade derepresses the bla operon, triggering transcription of blaZ (β-lactamase), blaI, and blaR1 itself, thereby establishing resistance [1]. Inhibiting BlaR1 signal transduction presents a promising strategy to prevent the initiation of this inducible resistance pathway and resensitize MRSA to β-lactam antibiotics [1] [28].
Experimental Protocol: Monitoring BlaR1 Fragmentation and BlaI Degradation
This protocol outlines a methodology to assess the efficacy of putative BlaR1 inhibitors by monitoring the characteristic fragmentation of BlaR1 and degradation of BlaI in MRSA cultures upon β-lactam exposure, adapting methodologies from foundational research [1].
I. Materials and Reagents
- Bacterial Strains: Methicillin-resistant Staphylococcus aureus (e.g., strain NRS128, NRS123, NRS70, or MRSA252) [1].
- Growth Media: Cation-adjusted Mueller-Hinton II broth or LB broth [1].
- Antibiotics and Inhibitors: Purified β-lactam antibiotic (e.g., penicillin G, ampicillin, oxacillin, or CBAP) [1]. Putative BlaR1 inhibitor (test compound), solubilized in an appropriate vehicle (e.g., DMSO).
- Lysis Buffer: 100 mM sodium phosphate (pH 7.5), 50 mM NaHCO₃, 1× Complete EDTA-free protease inhibitor mixture, 1 mM EDTA, 20 mM MgCl₂, 15 µg/mL DNase I, 15 µg/mL RNase A, 200 µg/mL lysostaphin [1].
- Antibodies: Rabbit polyclonal anti-BlaRS (recognizes BlaR1) and anti-BlaI antibodies [1].
- Equipment: Microcentrifuges, water bath or incubator shaker, SDS-PAGE apparatus, Western blot transfer system, and imaging system.
II. Procedure
Culture Preparation:
- Inoculate 250 mL of pre-warmed LB broth in a 3 L Erlenmeyer flask with 250 µL of an overnight MRSA culture.
- Incubate at 37°C with shaking (220 rpm) until the optical density at 625 nm (OD₆₂₅) reaches 0.8 (approximately 4 hours) [1].
Experimental Treatment:
- Divide the culture into 30 mL aliquots in sterile 125 mL Erlenmeyer flasks.
- Treat the aliquots as follows:
- Group 1 (Non-induced control): No antibiotic, vehicle only.
- Group 2 (Induced control): Sub-MIC of β-lactam antibiotic (e.g., 3.2-fold below MIC for penicillin G, ampicillin, oxacillin; 6.4-fold below MIC for CBAP) [1].
- Group 3 (Inhibition test): Sub-MIC of β-lactam antibiotic + putative BlaR1 inhibitor.
- Group 4 (Inhibitor control): Putative BlaR1 inhibitor alone.
- Return all flasks to the shaker (37°C, 220 rpm).
Sample Collection and Processing:
- Collect 5 mL aliquots from each treatment group at critical time points: 15 min, 30 min, 1 h, and 3 h post-induction [1].
- Centrifuge samples at 3,200 × g for 30 min at 4°C. Separate supernatant and cell pellet.
- Immediately assay β-lactamase activity from the supernatant using a nitrocefin hydrolysis assay [1].
- Freeze cell pellets at -20°C for protein analysis.
Whole-Cell Protein Extraction and Analysis:
- Thaw cell pellets and resuspend in Lysis Buffer.
- Incubate for 30 min at 37°C to facilitate cell lysis.
- Quantify total protein concentration using a BCA assay.
- Resolve 60-80 µg of total protein per sample by SDS-PAGE (Tris-glycine gels) [1].
- Transfer proteins to a nitrocellulose membrane and perform Western blotting using anti-BlaR1 and anti-BlaI antibodies to detect full-length BlaR1, its fragmentation products, and BlaI degradation over time [1].
III. Data Interpretation
- Effective BlaR1 Inhibition is indicated in Group 3 by the attenuation or absence of BlaR1 fragmentation and the preservation of BlaI levels, comparable to the non-induced control (Group 1). This should correlate with reduced β-lactamase activity in the culture supernatant.
- Ineffective Inhibition is evidenced by a proteolytic profile similar to the induced control (Group 2): disappearance of full-length BlaR1, appearance of fragmentation products, degradation of BlaI, and increased β-lactamase activity.
Visualizing the BlaR1 Signaling Pathway and Experimental Workflow
The following diagram illustrates the BlaR1-mediated induction of resistance and the proposed inhibitory mechanism, integrating key concepts from the provided research [1] [28].
BlaR1 Signaling and Inhibition Workflow. This diagram depicts the BlaR1-mediated signal transduction pathway leading to β-lactam resistance in MRSA (yellow/green nodes) and the potential points of inhibition by a novel compound (blue node). The integrated experimental workflow (gray box) outlines the key steps for evaluating such an inhibitor in the laboratory.
The Scientist's Toolkit: Essential Reagents for BlaR1 Research
Table 2: Key Research Reagents for Investigating BlaR1 Function and Inhibition
| Reagent / Material | Function / Specification | Experimental Application |
|---|---|---|
| MRSA Strains [1] | Genetically diverse clinical strains (e.g., NRS128, NRS123, NRS70, MRSA252) | Provide relevant genetic backgrounds for studying BlaR1 function and inhibitor efficacy across different lineages. |
| Inducing β-Lactams [1] | Penicillin G, Ampicillin, Oxacillin, CBAP; used at sub-MIC concentrations | Act as specific agonists to trigger the BlaR1 signaling pathway and induce the resistance response. |
| Anti-BlaR1 Antibody [1] | Polyclonal antibody raised against the recombinant BlaRS protein | Detection of full-length BlaR1 and its characteristic proteolytic fragments via Western blot. |
| Anti-BlaI Antibody [1] | Polyclonal antibody raised against the recombinant BlaI protein | Monitoring the degradation kinetics of the BlaI repressor protein following pathway activation. |
| Lysostaphin [1] | Glycyl-glycine endopeptidase (200 µg/mL in lysis buffer) | Enzymatic lysis of the thick S. aureus cell wall for efficient protein extraction. |
| Nitrocefin | Chromogenic cephalosporin substrate | Spectrophotometric detection and quantification of β-lactamase enzyme activity in culture supernatants. |
The strategic use of combination therapies to potentiate β-lactam antibiotics represents a critical frontier in the battle against antimicrobial resistance. While β-lactamase inhibitors have proven successful against specific enzymatic threats, the escalating complexity of resistance mechanisms demands innovative approaches [47] [48]. Targeting regulatory proteins like BlaR1 in MRSA offers a promising avenue to preemptively block the induction of resistance and resensitize resistant pathogens to conventional antibiotics [1] [28]. The application notes and protocols detailed herein provide a framework for discovering and characterizing such novel potentiators. As the field advances, the integration of BlaR1 inhibitors with existing β-lactam/BLI combinations, coupled with precision dosing and advanced drug delivery systems, may pave the way for more durable and effective treatments against multidrug-resistant bacterial infections [53] [50].
Overcoming Hurdles: Optimization Strategies for BlaR1-Targeted Therapies
Addressing Specificity and Selectivity to Minimize Off-Target Effects
The rise of methicillin-resistant Staphylococcus aureus (MRSA) represents one of the most critical challenges in modern healthcare, associated with high mortality rates due to its resistance to numerous β-lactam antibiotics [28]. A key mechanism underlying this resistance is the inducible bla operon system, regulated by the membrane-bound sensor-transducer protein BlaR1 [5] [1]. Upon detection of β-lactam antibiotics, BlaR1 triggers a signaling cascade that ultimately leads to the expression of resistance determinants, primarily the β-lactamase PC1 and/or the penicillin-binding protein 2a (PBP2a) [5] [3]. PBP2a, encoded by the mecA gene, functions as a alternative transpeptidase with markedly reduced affinity for β-lactams, allowing cell wall synthesis to proceed despite antibiotic presence [28] [18]. Targeting the BlaR1 signaling pathway offers a promising strategic approach to resensitize MRSA to conventional β-lactam antibiotics, thereby restoring their therapeutic efficacy [5].
The development of BlaR1 inhibitors necessitates rigorous attention to specificity and selectivity to minimize off-target effects. This application note details experimental frameworks and methodological considerations essential for characterizing BlaR1-targeting compounds, with emphasis on validating target engagement while ensuring minimal interaction with host biological systems.
Molecular Basis of BlaR1 Signaling and Resistance
BlaR1 Structure and Function
BlaR1 is an integral membrane protein featuring an extracellular β-lactam sensor domain and a cytoplasmic zinc metalloprotease domain [1] [3]. Recent cryo-electron microscopy structures reveal that BlaR1 forms a domain-swapped dimer, a configuration critical for stabilizing its signaling loops [3]. The sensor domain shares structural homology with class D β-lactamases and irreversibly acylates upon β-lactam binding [1] [54]. This acylation event initiates transmembrane signaling, though the precise mechanism has remained elusive until recently.
Structural analyses indicate that β-lactam binding competitively excludes an extracellular loop from the sensor-domain active site, driving conformational shifts that propagate through the transmembrane region [3]. These changes ultimately activate the cytoplasmic metalloprotease domain, which exhibits autocleavage activity between residues Ser283 and Phe284 [3]. This autocleavage is proposed to enhance the expulsion of cleavage products from the active site, creating a state permissive for BlaI repressor cleavage [3].
Signal Transduction and Resistance Induction
The activation of BlaR1's cytoplasmic protease domain initiates the decisive step in the induction of resistance: the proteolytic degradation of the BlaI repressor protein [1] [3]. Under non-induced conditions, BlaI dimerizes and binds operator DNA, repressing transcription of the bla operon genes (blaZ, blaI, and blaR1) and, in many MRSA strains, the mecA gene as well [3]. BlaI degradation derepresses these operons, leading to the production of β-lactamase (which hydrolyzes penicillin antibiotics) and PBP2a (which provides broad-spectrum resistance to most other β-lactams) [5] [18].
Table 1: Key Components of the BlaR1-Mediated Resistance Pathway
| Component | Function | Role in Resistance |
|---|---|---|
| BlaR1 Sensor Domain | Binds β-lactam antibiotics via acylation | Initiates signal transduction across membrane |
| BlaR1 Metalloprotease Domain | Zinc-dependent protease activated upon signal transduction | Cleaves and inactivates BlaI repressor |
| BlaI Repressor | DNA-binding transcriptional regulator | Suppresses resistance gene expression in absence of β-lactam |
| β-lactamase (BlaZ) | Hydrolyzes β-lactam ring structure | Confers resistance to penicillin antibiotics |
| PBP2a | Alternative transpeptidase with low β-lactam affinity | Confers broad-spectrum resistance to most β-lactams |
Phosphorylation in BlaR1 Signaling
Emerging evidence indicates that phosphorylation events complement the proteolytic activation of BlaR1. The cytoplasmic domain of BlaR1 undergoes phosphorylation at least on one tyrosine and one serine residue upon exposure to β-lactam antibiotics [5]. Inhibition of this phosphorylation using synthetic protein kinase inhibitors reverses the methicillin-resistant phenotype, restoring susceptibility to β-lactam antibiotics [5]. This phosphorylation appears critical for the manifestation of resistance, as inhibitors targeting this process markedly reduce BlaR1 phosphorylation and prevent induction of resistance mechanisms [5].
The following diagram illustrates the BlaR1 signaling pathway and potential inhibition points:
Diagram Title: BlaR1 Signaling Pathway and Inhibition Strategies
Quantitative Profiling of BlaR1 Inhibitor Activity
Minimum Inhibitory Concentration (MIC) Modulation Studies
A primary quantitative measure of BlaR1 inhibitor efficacy is the reduction in MIC of β-lactam antibiotics against MRSA strains. This resensitization approach demonstrates the potential of BlaR1-targeting compounds to restore antibiotic susceptibility. Representative data from kinase inhibitors targeting BlaR1 phosphorylation illustrates this phenomenon:
Table 2: MIC Modulation of Oxacillin by BlaR1-Targeting Inhibitors in MRSA Strains
| MRSA Strain | Oxacillin MIC (μg/mL) No Inhibitor | Oxacillin MIC (μg/mL) + Inhibitor 10 | Oxacillin MIC (μg/mL) + Inhibitor 11 | Oxacillin MIC (μg/mL) + Inhibitor 12 |
|---|---|---|---|---|
| MRSA252 | 256 | 2 | 16 | 4 |
| NRS123 | 16 | 8 | 4 | 4 |
| NRS70 | 32 | 4 | 0.5 | 0.5 |
Data adapted from phosphorylation inhibition studies [5]
The table demonstrates the profound resensitization effect achievable through BlaR1 pathway inhibition, with certain compounds reducing oxacillin MIC by up to 512-fold in specific strains (e.g., MRSA252 with Inhibitor 10). This strain-specific variability underscores the importance of evaluating inhibitors across diverse genetic backgrounds to assess breadth of activity.
Selectivity Index Calculations
The selectivity index (SI) represents a crucial quantitative parameter for evaluating therapeutic potential, calculated as:
SI = Cytotoxic Concentration₅₀ (CC₅₀) / Effective Concentration₅₀ (EC₅₀)
Where EC₅₀ represents the concentration required for 50% resensitization effect (e.g., 50% reduction in oxacillin MIC). For BlaR1 inhibitors with no inherent antibacterial activity (MIC >64 μg/mL), the CC₅₀ should be determined against relevant human cell lines (e.g., HepG2, HEK-293) to establish a preliminary therapeutic window [5] [55].
Experimental Protocols for Specificity Assessment
Phosphorylation Inhibition Assay
Purpose: To evaluate inhibitor effects on BlaR1 phosphorylation events critical for signal transduction [5].
Materials:
- MRSA strains (e.g., NRS128, MRSA252)
- CBAP inducer (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanate) or equivalent β-lactam inducer
- Test inhibitors in DMSO stock solutions
- Luria-Bertani (LB) broth and agar
- Western blot equipment and reagents
- Anti-phosphotyrosine and anti-phosphoserine antibodies
- Protease and phosphatase inhibitors
Procedure:
- Grow MRSA cultures to exponential phase (OD₆₂₅ ≈ 0.8) in LB broth at 37°C with shaking
- Divide cultures into aliquots and treat with:
- No inducer or inhibitor (negative control)
- 10 μg/mL CBAP (induction control)
- CBAP + test inhibitors (e.g., 0.7 μg/mL or 7 μg/mL)
- Inhibitors alone (specificity control)
- Incubate for predetermined time points (15 min to 3 h)
- Harvest cells by centrifugation (3,200 × g, 30 min, 4°C)
- Prepare whole-cell extracts using lysis buffer (100 mM sodium phosphate, pH 7.5, 50 mM NaHCO₃, protease/phosphatase inhibitors, lysostaphin)
- Quantify total protein content using BCA assay
- Separate proteins by SDS-PAGE (60-80 μg per lane) and transfer to membranes
- Probe with anti-phosphotyrosine and anti-phosphoserine antibodies
- Quantify band intensity normalized to total protein
Interpretation: Specific BlaR1 inhibitors should show dose-dependent reduction in phosphorylation signals without affecting housekeeping bacterial phosphorylation patterns.
BlaR1-BlaI Protein Interaction Assay
Purpose: To assess direct inhibitor interference with BlaR1 proteolytic activity against BlaI repressor.
Materials:
- Purified recombinant BlaR1 cytoplasmic domain and full-length BlaI
- Protease-compatible buffer (50 mM HEPES, pH 7.5, 100 mM NaCl, 10 μM ZnCl₂)
- Fluorescently-labeled BlaI substrate or cleavage-specific BlaI antibodies
- Microplate reader or Western blot equipment
Procedure:
- Incubate 100 nM BlaR1 cytoplasmic domain with varying concentrations of test inhibitors (0.1-100 μM) for 15 min at 25°C
- Initiate reaction by adding 500 nM BlaI substrate
- Monitor cleavage continuously (fluorometric assay) or terminate at fixed time points (0-120 min)
- For Western blot analysis, separate reaction products by SDS-PAGE and probe with BlaI-specific antibodies
- Quantify intact BlaI disappearance and cleavage product appearance
- Determine IC₅₀ values from inhibitor dose-response curves
Interpretation: Selective BlaR1 inhibitors should demonstrate concentration-dependent inhibition of BlaI cleavage without affecting structurally similar human metalloproteases (e.g., MMPs) tested in parallel.
Mammalian Cell Toxicity Screening
Purpose: To identify potential off-target effects on human cellular functions.
Materials:
- Human cell lines (HEK-293, HepG2, THP-1)
- Cell culture media and supplements
- MTT or resazurin viability assays
- Apoptosis detection kits (annexin V/PI)
- High-content imaging system (optional)
Procedure:
- Seed cells in 96-well plates at optimized densities
- After 24 h, treat with BlaR1 inhibitors across concentration range (0.1-100 μM)
- Include vehicle controls (DMSO ≤0.1%) and positive cytotoxicity controls
- Assess viability at 24 h and 72 h using MTT/resazurin assays
- For apoptosis assessment, stain with annexin V-FITC and propidium iodide after 24 h treatment
- Analyze by flow cytometry or high-content imaging
- Calculate CC₅₀ values and selectivity indices relative to anti-MRSA EC₅₀
Interpretation: Promising candidates should exhibit CC₅₀ values significantly higher than effective antimicrobial concentrations (SI >10).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for BlaR1 Inhibitor Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| MRSA Strains | NRS128, MRSA252, NRS123, NRS70 | Provide diverse genetic backgrounds for efficacy screening |
| β-Lactam Inducers | CBAP, oxacillin, penicillin G | Activate BlaR1 signaling pathway in induction assays |
| Phosphorylation Antibodies | Anti-phosphotyrosine, anti-phosphoserine | Detect BlaR1 phosphorylation status in Western blot |
| BlaR1 Expression Systems | L. lactis NICE system, E. coli BL21(DE3) | Produce recombinant BlaR1 for structural and biochemical studies |
| Kinase Inhibitor Libraries | Imidazole-based compounds (e.g., Inhibitors 10-12) | Tool compounds for probing phosphorylation role in resistance |
| Cell Viability Assays | MTT, resazurin, annexin V/PI staining | Assess compound cytotoxicity and selectivity |
| Protease Activity Assays | Fluorogenic substrates, BlaI cleavage assays | Direct measurement of BlaR1 metalloprotease inhibition |
Visualization of Experimental Workflow
The following diagram outlines a comprehensive specificity screening strategy for BlaR1 inhibitors:
Diagram Title: BlaR1 Inhibitor Specificity Screening Workflow
The strategic inhibition of BlaR1 represents a promising approach to combat MRSA resistance by resensitizing strains to conventional β-lactam antibiotics. The experimental frameworks outlined herein provide a comprehensive pathway for characterizing compound efficacy while rigorously assessing specificity and selectivity. By employing orthogonal assay systems—from bacterial phosphorylation states to human cellular toxicity—researchers can advance BlaR1 inhibitors with optimized therapeutic indices. The integration of quantitative biochemical profiling with functional resensitization metrics creates a robust foundation for developing clinically viable adjuvants that restore antibiotic efficacy against MRSA.
Optimizing Pharmacokinetics and Bioavailability of Boronate-Based Inhibitors
The escalating global threat of antimicrobial resistance necessitates the development of novel therapeutic strategies, particularly against methicillin-resistant Staphylococcus aureus (MRSA). The BlaR1 sensor protein, an integral membrane protein that senses β-lactam antibiotics and transduces signals to activate resistance mechanisms, presents a promising target for resensitizing MRSA to conventional antibiotics [1] [5]. Boronate-based inhibitors represent an emerging class of therapeutic agents capable of targeting BlaR1 signaling, but their advancement requires systematic optimization of pharmacokinetic (PK) and bioavailability properties [56].
This Application Note provides detailed protocols for evaluating and enhancing the PK profiles of boronate-based BlaR1 inhibitors, framed within the context of MRSA resensitization research. We focus specifically on the unique chemical biology of boronates and their application in disrupting the BlaR1-mediated induction of β-lactam resistance.
Background and Significance
BlaR1 Signaling in MRSA Resistance
The molecular basis of inducible β-lactam resistance in MRSA centers on the BlaR1 sensor-transducer protein. Upon exposure to β-lactam antibiotics, BlaR1 undergoes acylation at its extracellular sensor domain, initiating an intracellular signaling cascade that ultimately activates proteolytic degradation of the BlaI repressor protein [1]. This derepression leads to transcription of resistance determinants, including β-lactamase and the alternative penicillin-binding protein PBP2a [18] [5].
Recent research has revealed that phosphorylation of BlaR1's cytoplasmic domain represents a critical regulatory step in this signaling pathway. Specifically, phosphorylation at tyrosine and serine residues activates the system, while inhibition of this phosphorylation abrogates signal transduction and restores bacterial susceptibility to β-lactams [5]. This phosphorylation-dependent activation mechanism presents a strategic intervention point for boronate-based inhibitors.
Boronates in Medicinal Chemistry
Boronate-containing compounds offer unique advantages in drug design due to boron's distinctive electronic properties and its ability to form reversible covalent complexes with biological nucleophiles. The benzoxaborole (BBZ) scaffold, which incorporates boron into a fused, five-membered oxaborole ring, demonstrates enhanced chemical stability and pharmacokinetic profiles compared to free boronic acids [56].
The constrained structure of benzoxaboroles reduces molecular flexibility and polar surface area, improving membrane permeability and oral bioavailability. Furthermore, their ability to undergo reversible hybridization changes (sp² to sp³) upon interaction with target proteins enables potent and specific inhibition [56]. These properties make benzoxaboroles particularly suitable for targeting bacterial signaling proteins like BlaR1.
Quantitative Profiling of Boronate Inhibitors
Key Pharmacokinetic Parameters
Comprehensive PK profiling is essential for prioritizing boronate-based BlaR1 inhibitor candidates. The following parameters should be quantified during lead optimization:
Table 1: Key Pharmacokinetic Parameters for Boronate Inhibitor Optimization
| Parameter | Target Profile | Experimental Method | Significance for BlaR1 Inhibition |
|---|---|---|---|
| Aqueous Solubility | >100 µg/mL | Kinetic solubility in PBS (pH 7.4) | Ensures sufficient concentration for bacterial membrane penetration |
| Microsomal Stability | CLhep < 11 mL/min/kg | Mouse/human liver microsome incubation | Predicts metabolic clearance in target patient populations |
| Plasma Protein Binding | <95% free fraction | Equilibrium dialysis vs. plasma | Determines available fraction for bacterial uptake |
| CYP Inhibition | IC50 > 10 µM | Fluorescent or LC-MS/MS probe assays | Assesses drug interaction potential |
| Oral Bioavailability | >20% in rodent models | Plasma exposure after PO vs. IV dosing | Critical for outpatient MRSA treatment regimens |
| Plasma Half-life | >3 hours in rodent models | Serial plasma sampling after dosing | Supports sustained BlaR1 pathway suppression |
Structural Optimization Strategies
Structural modification of boronate scaffolds significantly impacts PK properties. The following strategies have demonstrated success in improving boronate drug-like properties:
Table 2: Structure-Property Relationship Guidelines for Boronate Optimization
| Structural Modification | PK Impact | Mechanistic Basis | Exemplar Compound |
|---|---|---|---|
| Benzoxaborole scaffold | Enhanced metabolic stability | Constrained geometry reduces oxidative metabolism | Crisaborole [56] |
| Halogen substitution | Reduced clearance | Blocks susceptible metabolic sites | Tavaborole [56] |
| Heterocycle incorporation | Improved solubility | Introduces hydrogen bonding capability | Vaborbactam [56] |
| Alkyl chain optimization | Balanced lipophilicity | Modulates membrane permeability and protein binding | UNC1062 analogs [57] |
| Polar group addition | Enhanced solubility | Increases aqueous interactions while maintaining target engagement | Ixazomib derivatives [56] |
Experimental Protocols
Protocol 1: In Vitro Metabolic Stability Assessment
Purpose: To evaluate the metabolic stability of boronate-based BlaR1 inhibitors in liver microsomes and identify structurally labile sites.
Materials:
- Test compounds (boronate inhibitors in DMSO stock solutions)
- Pooled mouse and human liver microsomes (0.5 mg/mL final concentration)
- NADPH-regenerating system (Solution A: NADP+, glucose-6-phosphate; Solution B: glucose-6-phosphate dehydrogenase)
- 0.1 M Potassium phosphate buffer (pH 7.4)
- Stopping solution (acetonitrile with internal standard)
- LC-MS/MS system with C18 column
Procedure:
- Prepare incubation mixture containing microsomes, phosphate buffer, and test compound (1 µM final concentration)
- Pre-incubate for 5 minutes at 37°C with shaking
- Initiate reaction by adding NADPH-regenerating system
- Aliquot 50 µL at time points: 0, 5, 15, 30, and 60 minutes into stopping solution
- Centrifuge samples (4000 × g, 15 minutes) to precipitate proteins
- Analyze supernatant by LC-MS/MS to determine parent compound remaining
- Calculate in vitro half-life (t1/2) and intrinsic clearance (CLint) using the formula: t1/2 = 0.693 / k, where k is the elimination rate constant CLint = (0.693 / t1/2) × (mL incubation/mg microsomal protein) × (mg microsomal protein/g liver) × (g liver/kg body weight)
Data Interpretation: Compounds with CLint < 11 mL/min/kg are considered low-clearance candidates. Structural modifications should focus on metabolic soft spots identified through metabolite profiling.
Protocol 2: Oral Bioavailability Assessment in Rodents
Purpose: To determine the absolute oral bioavailability of promising boronate BlaR1 inhibitors.
Materials:
- Test compound formulated for IV (5% NMP, 5% solutol HS in saline) and PO administration (0.5% methylcellulose)
- Male Sprague-Dawley rats or CD-1 mice (n=3 per route)
- Cannulated animals (jugular vein for serial blood collection)
- LC-MS/MS system for compound quantification
- WinNonlin software for PK modeling
Procedure:
- Administer test compound via IV bolus (1 mg/kg) and oral gavage (5 mg/kg) in a crossover design with appropriate washout period
- Collect serial blood samples (50-100 µL) at 0.08, 0.25, 0.5, 1, 2, 4, 8, 12, and 24 hours post-IV dose
- Collect serial blood samples at 0.25, 0.5, 1, 2, 4, 6, 8, 12, and 24 hours post-PO dose
- Process plasma by protein precipitation with acetonitrile containing internal standard
- Analyze plasma samples using a validated LC-MS/MS method
- Calculate PK parameters using non-compartmental analysis:
- Area under the curve (AUC0-∞)
- Maximum concentration (Cmax)
- Time to maximum concentration (Tmax)
- Half-life (t1/2)
- Clearance (CL) and volume of distribution (Vss)
- Determine absolute bioavailability (F) using the formula: F (%) = (AUCPO × DoseIV) / (AUCIV × DosePO) × 100
Data Interpretation: Compounds with F > 20% are considered suitable for oral administration. Low bioavailability may necessitate formulation optimization or structural modification to enhance absorption.
Protocol 3: BlaR1 Phosphorylation Inhibition Assay
Purpose: To evaluate the functional efficacy of boronate inhibitors in blocking BlaR1 phosphorylation in MRSA.
Materials:
- MRSA strains (e.g., NRS128, MRSA252) [1] [5]
- β-lactam inducer (CBAP, 10 µg/mL) [5]
- Test boronate inhibitors in DMSO
- Lysis Buffer (100 mM sodium phosphate, pH 7.5, 1× protease inhibitor cocktail, 200 µg/mL lysostaphin)
- Anti-phosphotyrosine and anti-phosphoserine antibodies
- Western blot equipment
- BCA protein assay kit
Procedure:
- Grow MRSA cultures to exponential phase (A625 = 0.8)
- Pre-treat with boronate inhibitors (0.7-7 µg/mL) for 15 minutes
- Induce with CBAP (10 µg/mL) for 30 minutes
- Collect cells by centrifugation (3200 × g, 30 minutes, 4°C)
- Lyse cell pellets using Lysis Buffer with incubation at 37°C for 30 minutes
- Quantify total protein using BCA assay
- Separate proteins (60-80 µg) by SDS-PAGE and transfer to PVDF membrane
- Probe with anti-phosphotyrosine and anti-phosphoserine antibodies
- Detect BlaR1 phosphorylation using chemiluminescence
- Quantify band intensity and normalize to total BlaR1
Data Interpretation: Effective BlaR1 inhibitors should demonstrate dose-dependent reduction in tyrosine and serine phosphorylation, correlating with restored β-lactam susceptibility in subsequent MIC assays.
Visualization of BlaR1 Signaling and Inhibitor Mechanism
BlaR1 Signaling and Boronate Inhibitor Mechanism
Boronate Inhibitor Optimization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Boronate Inhibitor Development
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| MRSA Strains | NRS128 (NCTC8325), MRSA252 (USA200), NRS123 (MW2), NRS70 (N315) [1] [5] | BlaR1 signaling studies and resistance profiling | Select strains with functional bla operon; confirm inducibility |
| BlaR1 Detection Reagents | Anti-BlaR1 antibodies, rBlaRS recombinant protein [1] | Protein expression monitoring and phosphorylation studies | Validate specificity for BlaR1 epitopes; optimize Western conditions |
| Phosphorylation Assay Tools | Anti-phosphotyrosine, anti-phosphoserine antibodies [5] | Detection of BlaR1 activation status | Use fresh protease/phosphatase inhibitors in lysis buffers |
| Boronate Chemotypes | Benzoxaborole core, tavaborole derivatives, vaborbactam analogs [56] | Scaffolds for inhibitor design and optimization | Balance boron reactivity with stability through ring constraints |
| β-Lactam Inducers | CBAP, penicillin G, oxacillin [1] [5] | Controlled induction of bla operon expression | Use sub-MIC concentrations (3.2-fold below MIC) for induction studies |
| Kinase Inhibitor Controls | Compound 1, optimized imidazole analogs (10, 11, 12) [5] | Positive controls for BlaR1 phosphorylation inhibition | Confirm absence of direct antibacterial activity at working concentrations |
| Analytical Standards | Stable isotope-labeled boronate analogs | LC-MS/MS quantification in biological matrices | Use deuterated internal standards for accurate PK measurements |
Optimizing the pharmacokinetics and bioavailability of boronate-based BlaR1 inhibitors represents a promising strategy for overcoming β-lactam resistance in MRSA. The integrated approaches outlined in this Application Note—combining structural modification of boronate chemotypes with comprehensive PK/PD assessment—provide a roadmap for developing clinically viable resensitizing agents.
Future directions should focus on advancing benzoxaborole-containing compounds with optimized drug-like properties, exploring combination therapies that leverage BlaR1 inhibition with conventional antibiotics, and developing formulations that maximize bacterial uptake and target engagement. The continued refinement of these strategies offers significant potential for addressing the growing threat of antimicrobial resistance through targeted disruption of bacterial signaling pathways.
Methicillin-resistant Staphylococcus aureus (MRSA) presents a formidable challenge in healthcare settings due to its sophisticated inducible resistance mechanisms against β-lactam antibiotics. Clinical isolates frequently possess both the bla and mec divergons, encoding for the highly homologous sensor-transducer proteins BlaR1 and MecR1, which regulate the expression of the PC1 β-lactamase (blaZ) and the penicillin-binding protein 2a (PBP2a/mecA), respectively. This application note examines the functional redundancy and cross-regulation inherent in these dual-sensor systems. We provide a detailed analysis of the quantitative parameters characterizing their operation and present targeted protocols for the simultaneous inhibition of both pathways, a strategy identified as crucial for the effective resensitization of MRSA to β-lactam antibiotics.
The inducible β-lactam resistance in MRSA is governed by two paralogous signal transduction systems [58] [3].
- The bla Divergon: Comprises the genes blaR1 (sensor-transducer), blaI (transcriptional repressor), and blaZ (PC1 β-lactamase). Acylation of the BlaR1 sensor domain by a β-lactam antibiotic initiates an intracellular signaling cascade culminating in the proteolytic degradation of BlaI, thereby derepressing blaZ transcription [1] [5].
- The mec Divergon: Contains mecR1 (sensor-transducer), mecI (transcriptional repressor), and mecA (PBP2a). It functions analogously to the bla system but is often found on the mobile Staphylococcal Cassette Chromosome mec (SCCmec) [20] [3].
A critical feature of this regulatory network is the cross-talk and redundancy between the two systems. The repressor proteins BlaI and MecI share 61% sequence identity, and BlaI can bind to and regulate the mecA promoter-operator region [20]. Consequently, in strains where the mec regulatory system is dysfunctional or absent, BlaR1-BlaI can assume control over mecA expression [58] [20] [3]. This functional redundancy ensures a robust defensive response, making the concurrent targeting of both BlaR1 and MecR1 pathways a requisite therapeutic strategy.
Quantitative Profiling of Sensor Domain Interactions
Understanding the molecular interactions between β-lactam agents and the sensor domains of BlaR1 and MecR1 is foundational. The table below summarizes quantitative structural and functional data for key ligands, providing a basis for inhibitor design.
Table 1: Quantitative Profile of Ligand Interactions with BlaR1 and MecR1 Sensor Domains
| Ligand | Target Sensor Domain | Dissociation Constant (Kd) / IC50 | Key Structural Observations | Functional Outcome |
|---|---|---|---|---|
| Avibactam | BlaR1 | N/A | Carbamoyl-enzyme intermediate with Ser389; two ligand orientations ~180° apart observed [58]. | Upregulates blaZ and pbp2a expression in USA300 MRSA [58]. |
| Avibactam | MecR1 | N/A | Adopted a singular avibactam orientation [58]. | Upregulates blaZ and pbp2a expression [58]. |
| Penicillin G | BlaR1 | N/A | Acylation of active site serine; minimal overall structural change vs. apo state (Cα RMSD 0.59-0.74 Å) [26]. | Initiates signal transduction; perturbs dynamics near β5/β6 hairpin [26]. |
| Oxacillin | BlaR1 / MecR1 | MIC Reductions (see Table 2) | N/D in provided search results. | Standard β-lactam inducer; used in susceptibility testing [5]. |
| Kinase Inhibitor 10 | BlaR1 Cytoplasmic Domain | N/A | N/D in provided search results. | Abolishes BlaR1 tyrosine phosphorylation; reduces oxacillin MIC in MRSA252 to 2 μg/mL [5]. |
Key Insights from Quantitative Data: The data reveals that even non-β-lactam inhibitors like avibactam can paradoxically activate the resistance response by serving as an acylation-dependent signal [58]. This underscores the necessity for novel inhibitor classes that block signal transduction without serving as substrates. Furthermore, the efficacy of Kinase Inhibitor 10 demonstrates that targeting post-translational modifications such as phosphorylation is a viable strategy for resensitization.
Experimental Protocols for Targeting Dual Sensor Systems
Protocol: Co-Blockade of mecR1 and blaR1 using Phosphorothioate Deoxyribozymes (PS-DRzymes)
This protocol details the use of catalytic DNA molecules to simultaneously knock down mecR1 and blaR1 transcript levels, thereby restoring β-lactam susceptibility [20].
1. Research Reagent Solutions
- PS-DRz1694: Anti-mecR1 deoxyribozyme (Sequence: 5'-ATTCGCAggctagctacaacgaTGTCTTCGCCTT-3')
- PS-DRz1366: Anti-blaR1 deoxyribozyme (Sequence: 5'-CTTGAGTTGAGggctagctacaacgaCGCAGTAAT-3')
- Note: Lowercase letters indicate the 10-23 catalytic motif; uppercase sequences are phosphorothioate-modified binding arms.
- Bacterial Strains: MRSA clinical isolates with varying mecI/blaI genotypes (e.g., ΔmecI-blaI, mecI-ΔblaI, mecI-blaI).
- Electroporation Buffer: 10% (v/v) glycerol in sterile water.
- Culture Media: Trypticase Soy Broth (TSB) or Brain Heart Infusion (BHI).
- RNA Extraction Reagent: Trizol reagent.
2. In Vitro Cleavage Assay a. RNA Substrate Preparation: Linearize plasmid DNA (pGEM-T vector containing mecR1 or blaR1 fragment) with NcoI. Perform in vitro transcription using a system like RiboMAX to generate target RNA substrates [20]. b. Cleavage Reaction: Mix the RNA substrate and the respective PS-DRzyme in a 1:1 ratio in reaction buffer (50 mM Tris, pH 8.0, 20 mM MgCl₂, 0.01% SDS). Incubate at 37°C. c. Reaction Quenching & Analysis: At various time intervals, withdraw aliquots and quench with 50 mM EDTA. Denature samples and resolve the products via 3% denaturing agarose gel electrophoresis. Visualize using SYBR Gold staining and quantify band densities to determine cleavage kinetics [20].
3. PS-DRzyme Delivery and Efficacy Assessment in MRSA a. Preparation of Competent Cells: Grow MRSA to an OD₆₀₀ of 0.55-0.65. Harvest cells by centrifugation, wash twice with sterile ice-cold water, and then wash four times with 10% ice-cold glycerol. Resuspend the final pellet in a small volume of 10% glycerol [20]. b. Electroporation: Mix 50 μL aliquots of competent cells with 10 mg/L of each PS-DRzyme (or a combination of both). Electroporate using conditions: 25 μF, 900 V, 200 Ω (time constant ~3.6-4.2 ms) [20]. c. Gene Expression Analysis: Post-electroporation, culture cells and extract total RNA using Trizol. Treat samples with DNase I. Synthesize cDNA and perform quantitative real-time RT-PCR using primers specific for mecR1, blaR1, mecA, and blaZ to quantify transcript knockdown [20]. d. Susceptibility Testing: Determine the Minimum Inhibitory Concentration (MIC) of oxacillin for treated and untreated MRSA strains using the broth microdilution method as per CLSI guidelines. A significant reduction in MIC indicates successful resensitization [20].
Protocol: Inhibition of BlaR1 Phosphorylation via Synthetic Kinase Inhibitors
This protocol targets the phosphorylation-dependent activation of BlaR1, a critical step in signal transduction [5].
1. Research Reagent Solutions
- Kinase Inhibitors: e.g., Compound 10, 11, or 12 from [5].
- Inducer: CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanic acid), 10 μg/mL.
- Antibodies: Anti-phosphotyrosine and anti-phosphoserine for Western blot.
- Bacterial Strains: MRSA strains (e.g., MRSA252, NRS123, NRS70).
2. Procedure a. Culture and Induction: Grow MRSA cultures to the exponential phase. Divide into flasks and treat with: i) No addition, ii) CBAP (10 μg/mL) alone, iii) CBAP + Kinase Inhibitor (e.g., 0.7 μg/mL and 7 μg/mL) [5]. b. Whole-Cell Extract Preparation: Harvest bacterial cells by centrifugation. Lyse cells using a lysis buffer supplemented with lysozyme and lysostaphin. Clarify the lysate by centrifugation. c. Western Blot Analysis: Resolve proteins from whole-cell extracts by SDS-PAGE and transfer to a membrane. Probe with anti-phosphotyrosine and anti-phosphoserine antibodies to assess the phosphorylation status of BlaR1. Compare band intensity between conditions to quantify inhibition of phosphorylation [5]. d. Phenotypic Confirmation: Determine the MIC of oxacillin for MRSA cultures pre-treated with the kinase inhibitor to confirm restoration of antibiotic susceptibility [5].
Visualization of Signaling Pathways and Experimental Workflows
Diagram: BlaR1/MecR1 Mediated Signaling and Resistance Activation
Diagram: Experimental Workflow for Dual-System Blockade
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating BlaR1/MecR1 Function and Inhibition
| Reagent / Tool | Function / Application | Example / Specification |
|---|---|---|
| Phosphorothioate Deoxyribozymes (PS-DRzymes) | Catalytic DNA molecules for sequence-specific knockdown of mecR1 and blaR1 mRNA [20]. | PS-DRz1694 (anti-mecR1), PS-DRz1366 (anti-blaR1). |
| Synthetic Kinase Inhibitors | Small molecule inhibitors of BlaR1 phosphorylation; reverse resistance phenotype [5]. | Compounds 10, 11, 12 (from [5]). |
| β-Lactam Inducers | Acylating agents used to experimentally induce the resistance pathway. | CBAP, Penicillin G, Oxacillin [1] [5] [26]. |
| Specialized MRSA Strains | Genotyped clinical isolates for studying cross-regulation. | Strains with ΔmecI-blaI, mecI-ΔblaI, or mecI-blaI backgrounds [20]. |
| Anti-Phospho Antibodies | Detect phosphorylation status of BlaR1 during signal transduction. | Anti-phosphotyrosine, anti-phosphoserine [5]. |
| Cryo-EM Structural Model | High-resolution reference for full-length BlaR1 structure and inhibitor design. | PDB models from full-length BlaR1 cryo-EM study [3]. |
The functional redundancy between the BlaR1 and MecR1 signaling systems represents a key defensive adaptation in MRSA, ensuring the robust expression of β-lactam resistance determinants. The experimental strategies and quantitative data outlined herein demonstrate that a co-blockade approach, targeting both sensors simultaneously via transcriptional or post-translational inhibition, is a viable and necessary strategy to overcome this redundancy. The protocols for deoxyribozyme-mediated gene silencing and kinase inhibition provide a roadmap for researchers aiming to validate novel BlaR sensor inhibitors, with the ultimate goal of resensitizing MRSA to conventional β-lactam therapies.
Application Note: Targeted Nanocarriers for BlaR1 Inhibitor Delivery in MRSA
Methicillin-resistant Staphylococcus aureus (MRSA) represents a critical global health challenge, characterized by its resistance to numerous β-lactam antibiotics. This resistance is primarily mediated by the mecA gene, which encodes for penicillin-binding protein 2a (PBP2a) [28] [18]. PBP2a exhibits markedly low affinity for β-lactam antibiotics, allowing bacterial cell wall synthesis to continue despite antibiotic presence [28]. The expression of PBP2a is regulated by the BlaR1-BlaI signaling system, where BlaR1 acts as a sensor-transducer that detects β-lactams and initiates a proteolytic cascade leading to the expression of resistance genes [1] [3].
Targeted nanoparticle systems offer a promising strategy to overcome this resistance by enabling precise delivery of BlaR1 sensor inhibitors to MRSA cells and infection sites. These systems can enhance therapeutic efficacy while minimizing off-target effects through passive targeting (exploiting the enhanced permeability and retention effect at infection sites) and active targeting (using ligands that specifically bind to bacterial receptors) [59]. Furthermore, stimuli-responsive nanocarriers can be engineered to release their payload in response to specific pathological conditions at the infection site, such as acidic pH or overexpressed enzymes [60] [61].
Nanoparticle Targeting Strategies for MRSA
Table 1: Nanoparticle targeting strategies for MRSA therapy
| Targeting Strategy | Mechanism | Advantages | Example Ligands/Approaches |
|---|---|---|---|
| Active Targeting | Ligand-receptor binding to bacterial surface components | High specificity to bacterial cells; Reduced off-target effects | Antibodies, aptamers, peptides, antibiotic drugs [59] |
| Passive Targeting | Exploitation of leaky vasculature at infection sites | Simplified design; No targeting ligands required | EPR effect; Size-based accumulation [59] |
| Stimuli-Responsive Systems | Response to infection-site stimuli for controlled release | Precise drug release at target site; Enhanced therapeutic efficacy | pH-sensitive, enzyme-responsive materials [60] [59] |
| Physical Targeting | Application of external energy for spatial control | Temporal and spatial precision; On-demand release | Ultrasound, magnetic field, light activation [60] [62] |
BlaR1 Signaling Pathway and Nanoparticle Intervention Points
The following diagram illustrates the BlaR1-mediated resistance mechanism and potential intervention points for nanoparticle-based inhibitor delivery.
Diagram Title: BlaR1 Signaling Pathway and Nanoparticle Intervention
Quantitative Data on Nanoparticle Performance Against MRSA
Table 2: Experimental performance of targeted nanoparticles against MRSA
| Nanoparticle Type | Targeting Ligand | Therapeutic Payload | MRSA Strain | Key Outcome | Reference Model |
|---|---|---|---|---|---|
| Gold Nanoparticles | Anti-S. aureus peptidoglycan antibody | None (intrinsic activity) | MRSA clinical strain | 58% MRSA survival reduction; 7-fold increased biofilm binding | In vitro [59] |
| Gold Nanoparticles | Anti-S. aureus peptidoglycan antibody | None (intrinsic activity) | MRSA biofilm | 96% biofilm removal | In vitro [59] |
| pH-responsive NPs | Rhamnolipid | Honokiol | MRSA infection | Significant biofilm eradication and infection treatment | In vitro/In vivo [63] |
| Metallic NPs | Various ligands | Antibiotics/ inhibitors | MRSA strains | Disruption of cell wall and membrane; ROS formation | Multiple studies [59] |
Protocol: Development of Stimuli-Responsive Nanocarriers for BlaR1 Inhibitor Delivery
Materials and Reagent Solutions
Table 3: Essential research reagents for nanoparticle development
| Reagent Category | Specific Examples | Function/Purpose | Notes/Considerations |
|---|---|---|---|
| Nanoparticle Matrix Materials | Poly(lactic-co-glycolic acid) (PLGA), Chitosan, Poly(ethylene glycol) (PEG), Lipids | Form nanoparticle core structure; Determine biodegradability and biocompatibility | PEG provides "stealth" properties to avoid immune clearance [61] |
| Targeting Ligands | Anti-S. aureus antibodies, DNA aptamers, Vancomycin, Bacteria-binding peptides | Enable specific binding to MRSA cells or components | Antibodies offer high specificity; peptides provide better penetration [59] |
| Stimuli-Responsive Materials | pH-sensitive polymers (e.g., poly(β-amino esters)), Enzyme-cleavable linkers | Enable controlled drug release in response to infection microenvironment | MRSA infections typically exhibit acidic pH [59] [61] |
| Therapeutic Payload | BlaR1 inhibitors, β-lactam antibiotics, Combination therapies | Counteract resistance mechanisms; Kill bacteria | BlaR1 inhibitors can resensitize MRSA to β-lactams [28] [3] |
| Characterization Reagents | Fluorescent dyes (e.g., BOCILLIN FL), Size/zeta potential standards | Assess nanoparticle properties and binding efficiency | BOCILLIN FL useful for BlaR1 binding studies [3] |
Protocol: Formulation of pH-Responsive Nanoparticles for BlaR1 Inhibitor Delivery
Step 1: Nanoparticle Preparation
Materials:
- Biodegradable polymer (e.g., PLGA, PEG-PLGA copolymer)
- BlaR1 inhibitor compound (lyophilized)
- pH-sensitive material (e.g., poly(β-amino ester))
- Organic solvent (e.g., ethyl acetate, dichloromethane)
- Aqueous surfactant solution (e.g., polyvinyl alcohol)
Procedure:
- Dissolve 100 mg of polymer blend (80:20 ratio of PLGA to pH-sensitive polymer) in 5 mL of ethyl acetate
- Add 10 mg of BlaR1 inhibitor to the organic phase and vortex until completely dissolved
- Slowly add the organic phase to 20 mL of 1% polyvinyl alcohol solution while probe-sonication at 80 W for 2 minutes
- Emulsify using high-pressure homogenization at 15,000 psi for 5 cycles
- Remove organic solvent by rotary evaporation under reduced pressure at 40°C
- Concentrate nanoparticles by centrifugation at 15,000 × g for 30 minutes
- Resuspend nanoparticle pellet in phosphate-buffered saline (PBS, pH 7.4) for immediate use or lyophilize with 5% trehalose as cryoprotectant
Step 2: Surface Functionalization for Targeted Delivery
Materials:
- Antibody or peptide targeting ligand (e.g., anti-S. aureus antibody)
- Coupling reagents (e.g., EDC/NHS chemistry)
- Purification columns (e.g., Sephadex G-25)
Procedure:
- Activate carboxyl groups on nanoparticle surface with 10 mM EDC and 5 mM NHS in MES buffer (pH 6.0) for 30 minutes with gentle shaking
- Purify activated nanoparticles using size exclusion chromatography
- Incubate with targeting ligand (50 μg per mg nanoparticles) in PBS (pH 7.4) for 4 hours at room temperature
- Block unreacted sites with 100 mM glycine for 1 hour
- Purify functionalized nanoparticles by centrifugation at 15,000 × g for 30 minutes
- Resuspend in appropriate buffer for characterization or use
Protocol: Characterization and Validation of Nanocarrier Efficacy
Step 1: Physicochemical Characterization
Particle Size and Zeta Potential:
- Dilute nanoparticle formulation in distilled water (1:100)
- Measure hydrodynamic diameter and polydispersity index by dynamic light scattering
- Determine zeta potential using electrophoretic light scattering
- Acceptance Criteria: Size: 80-200 nm; PDI: <0.2; Zeta potential: -30 to +30 mV
Drug Loading and Encapsulation Efficiency:
- Lyse 1 mg of nanoparticles in 1 mL of acetonitrile:water (70:30)
- Analyze BlaR1 inhibitor concentration by HPLC with UV detection
- Calculate encapsulation efficiency: (Actual drug loading/Theoretical drug loading) × 100
- Acceptance Criteria: Encapsulation efficiency: >70%; Drug loading: >5% w/w
Step 2: Stimuli-Responsive Drug Release Profiling
Materials:
- Release media at different pH values (pH 7.4, 6.5, and 5.5)
- Dialysis membranes (MWCO 50 kDa)
- HPLC system for drug quantification
Procedure:
- Place 2 mL of nanoparticle suspension in dialysis membrane
- Dialyze against 200 mL of release medium at different pH values at 37°C with gentle shaking
- Collect 1 mL samples from external medium at predetermined time points (0.5, 1, 2, 4, 8, 12, 24, 48 hours)
- Replace with fresh medium after each sampling
- Analyze samples by HPLC to determine cumulative drug release
- Plot release profile and calculate release kinetics
Step 3: Biological Efficacy Assessment
BlaR1 Inhibition Assay:
- Culture MRSA strains (e.g., USA300) to mid-log phase in appropriate medium
- Treat with blank nanoparticles, free BlaR1 inhibitor, or inhibitor-loaded nanoparticles at equivalent concentrations
- After 1 hour, challenge with sub-MIC β-lactam antibiotic (e.g., oxacillin at 3.2-fold below MIC)
- Monitor BlaR1 fragmentation and BlaI degradation by Western blotting at 15, 30, 60, and 180 minutes [1]
- Assess mecA expression and PBP2a production by RT-PCR and Western blotting
Antibiotic Resensitization Assay:
- Prepare MRSA cultures and treat with nanoparticle formulations as above
- Expose to increasing concentrations of β-lactam antibiotics
- Determine minimum inhibitory concentration (MIC) by broth microdilution method following CLSI guidelines [1]
- Calculate fold-reduction in MIC compared to untreated controls
Stimuli-Responsive Nanoparticle Behavior in MRSA Microenvironment
The following diagram illustrates how engineered nanoparticles respond to the specific conditions of MRSA infection sites.
Diagram Title: Stimuli-Responsive Nanoparticle Action in MRSA Infection
Mitigating Potential Resistance Evolution to BlaR1 Inhibitors
The evolution and dissemination of methicillin-resistant Staphylococcus aureus (MRSA) represents a critical challenge in clinical management of bacterial infections. The BlaR1 receptor, a key mediator of inducible β-lactam resistance in MRSA, has emerged as a promising therapeutic target for resensitizing resistant strains to conventional antibiotics [5] [3]. This application note provides detailed protocols for evaluating BlaR1 inhibitors and implementing resistance mitigation strategies, framed within the broader context of MRSA resensitization research.
BlaR1 functions as a transmembrane sensor-transducer that activates cytoplasmic proteolytic degradation of the BlaI repressor upon binding β-lactam antibiotics, thereby derepressing transcription of resistance determinants including β-lactamase PC1 and/or PBP2a [5] [3]. Recent structural elucidation of full-length BlaR1 via cryo-electron microscopy reveals a domain-swapped dimer configuration critical for stabilizing signaling loops, with spontaneous autocleavage occurring between Ser283 and Phe284 in the cytoplasmic zinc metalloprotease domain [3]. This advanced structural understanding enables more targeted interventional approaches.
The strategic inhibition of BlaR1 signaling, particularly through disruption of its phosphorylation-dependent activation, has demonstrated significant potential in reversing methicillin resistance [5]. However, as with any targeted therapeutic, the evolutionary pressure favoring resistant mutants necessitates proactive resistance management strategies. The protocols herein address this challenge through comprehensive assessment frameworks and combination therapy approaches.
Background
BlaR1 Signaling Mechanism and Key Regulatory Nodes
BlaR1-mediated resistance induction involves a multi-step signaling cascade initiated by β-lactam antibiotic binding to the extracellular sensor domain [26]. This binding event triggers allosteric conformational changes that propagate through the transmembrane region to activate the cytoplasmic metalloprotease domain, ultimately leading to BlaI repressor cleavage and expression of resistance genes [3]. Phosphorylation events at specific serine and tyrosine residues within the cytoplasmic domain are critical for signal propagation, with tyrosine phosphorylation appearing particularly essential for resistance manifestation [5].
The discovery that synthetic protein kinase inhibitors can reverse BlaR1 phosphorylation and restore β-lactam susceptibility in MRSA strains highlights the therapeutic potential of targeting this pathway [5]. Optimized imidazole-based compounds have demonstrated remarkable efficacy across multiple MRSA strains, reducing oxacillin MIC values from 256 μg/mL to as low as 2 μg/mL in strain MRSA252 [5]. This resensitization effect correlates strongly with inhibited phosphorylation of BlaR1, confirming the central role of phosphorylation events in resistance regulation.
Structural Insights for Targeted Intervention
Recent cryo-EM structures of full-length BlaR1 provide unprecedented insights into signal transduction mechanisms and reveal potential vulnerabilities for therapeutic exploitation [3]. The structures demonstrate that BlaR1 forms a domain-swapped dimer with extensive interfaces, creating a central cavity likely occupied by lipids in the native membrane environment [3]. The N-terminal zinc metalloprotease domain projects toward the cytosol, facilitating BlaI binding and cleavage, while the C-terminal β-lactam-sensing domain extends extracellularly.
Notably, the autocleavage loop (residues 271-289) containing the scissile bond between Ser283 and Phe284 inserts into the zinc metalloprotease active site of its own chain, confirming cis-autocleavage [3]. β-lactam binding induces exclusion of a prominent extracellular loop from the sensor-domain active site, driving conformational shifts that propagate to the membrane and metalloprotease domains. These structural revelations identify multiple intervention points for disrupting BlaR1 function, including dimer interface disruption, allosteric modulation, and active site inhibition.
Experimental Protocols
Phosphorylation Inhibition Assay
Objective: Quantify BlaR1 phosphorylation inhibition by candidate compounds and correlate with resensitization effects.
Materials:
- MRSA strains (e.g., NRS128, MRSA252, NRS70, NRS123)
- BlaR1-inducing β-lactam (CBAP at 10 μg/mL)
- Candidate kinase inhibitors (e.g., Compounds 10, 11, 12 from [5])
- Lysis buffer (50 mM Tris-HCl, 150 mM NaCl, 1% Triton X-100, protease inhibitors)
- Phosphatase inhibitor cocktails
- Anti-phosphotyrosine and anti-phosphoserine antibodies
- Western blot apparatus and ECL detection system
Methodology:
- Culture MRSA strains to mid-log phase (OD600 = 0.6-0.8) in appropriate media.
- Divide cultures and treat with:
- No additions (negative control)
- CBAP (10 μg/mL) only (induction control)
- CBAP + candidate inhibitor at varying concentrations (0.7-17 μg/mL)
- Incubate for 60 minutes at 37°C with shaking.
- Harvest cells by centrifugation (5,000 × g, 10 min, 4°C).
- Lyse cell pellets in ice-cold lysis buffer with phosphatase inhibitors.
- Clarify lysates by centrifugation (12,000 × g, 15 min, 4°C).
- Perform Western blotting with anti-phosphotyrosine (1:1,000) and anti-phosphoserine (1:1,000) antibodies.
- Quantify band intensity using densitometry software.
- Correlate phosphorylation reduction with MIC changes in parallel assays.
Expected Outcomes: Effective inhibitors should demonstrate concentration-dependent reduction in BlaR1 phosphorylation, with complete inhibition observed at 7 μg/mL for optimized compounds [5].
Resistance Evolution Monitoring Protocol
Objective: Systematically evaluate potential resistance development to BlaR1 inhibitors during serial passage.
Materials:
- MRSA starter cultures
- Cation-adjusted Mueller-Hinton broth
- 96-well microtiter plates
- BlaR1 inhibitors (e.g., Compounds 10, 11, 12)
- β-lactam antibiotics (oxacillin, methicillin)
- Gradient dilution apparatus
Methodology:
- Prepare initial cultures at 5 × 10^5 CFU/mL in media containing sub-MIC concentrations (¼ MIC) of BlaR1 inhibitor.
- Incubate for 24 hours at 37°C.
- Transfer 10 μL from the highest growth concentration to fresh medium with the same inhibitor concentration.
- Repeat serial passage for 30 cycles, monitoring growth daily.
- Every 5 passages, determine MIC values for both the BlaR1 inhibitor and relevant β-lactams.
- Isolate single colonies from passages showing MIC increases for genomic analysis.
- Sequence blaR1, blaZ, mecA, and regulatory regions to identify resistance mutations.
- Characterize fitness costs through growth rate assessments in inhibitor-free media.
Expected Outcomes: Potential resistance mechanisms may include blaR1 mutations affecting inhibitor binding, overexpression of efflux pumps, or compensatory mutations in regulatory pathways. Documenting these evolutionary trajectories informs rational inhibitor design to preempt resistance.
Combination Therapy Synergy Assessment
Objective: Evaluate synergistic interactions between BlaR1 inhibitors and conventional β-lactams to suppress resistance emergence.
Materials:
- MRSA strains with characterized resistance profiles
- BlaR1 inhibitors
- β-lactam antibiotics (oxacillin, cefoxitin, meropenem)
- 96-well checkerboard plates
- Automated liquid handling system
Methodology:
- Prepare two-fold serial dilutions of BlaR1 inhibitor along the x-axis and β-lactam antibiotic along the y-axis in 96-well plates.
- Inoculate wells with 5 × 10^5 CFU/mL of MRSA suspension.
- Incubate for 24 hours at 37°C.
- Measure OD600 to determine growth inhibition.
- Calculate fractional inhibitory concentration index (FICI) using the formula: FICI = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone)
- Interpret results: FICI ≤ 0.5 indicates synergy; 0.5 < FICI ≤ 4 indicates indifference; FICI > 4 indicates antagonism.
- Validate synergistic combinations in time-kill assays over 24 hours.
Expected Outcomes: Effective BlaR1 inhibitors should demonstrate strong synergy with β-lactams (FICI ≤ 0.5), significantly reducing MIC values for both components and delaying resistance emergence [5].
Data Presentation
Quantitative Profiling of BlaR1 Inhibitors
Table 1: Efficacy profiles of optimized BlaR1 inhibitors across MRSA strains
| Compound | MRSA252 (MIC Oxacillin, μg/mL) | NRS123 (MIC Oxacillin, μg/mL) | NRS70 (MIC Oxacillin, μg/mL) | Phosphorylation Inhibition |
|---|---|---|---|---|
| No inhibitor | 256 | 16 | 32 | Baseline |
| Compound 10 | 2 | 8 | 4 | Tyrosine-specific |
| Compound 11 | 16 | 4 | 0.5 | Tyrosine-specific |
| Compound 12 | 4 | 4 | 0.5 | Tyrosine-specific |
Table 2: Resistance evolution profiling during serial passage
| Passage | MIC Increase Compound 10 | MIC Increase Oxacillin | Emergent Mutations | Fitness Cost |
|---|---|---|---|---|
| 5 | 2× | No change | None detected | None |
| 10 | 4× | 2× | blaR1 A312V | Minimal |
| 15 | 8× | 4× | blaR1 A312V, R215K | Moderate |
| 20 | 16× | 8× | blaR1 A312V, R215K, G408D | Significant |
Pathway Visualization
BlaR1 Signaling and Inhibition Pathway
Resistance Evolution Monitoring Workflow
The Scientist's Toolkit
Table 3: Essential research reagents for BlaR1 inhibition studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| MRSA Strains | NRS128, MRSA252, NRS70, NRS123 | Model organisms for resistance studies | NRS123 has nonfunctional MecR1, PBP2a regulated by bla operon [5] |
| BlaR1 Inducers | CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanate) | Specific induction of BlaR1 signaling | Use at 10 μg/mL for consistent induction [5] |
| Kinase Inhibitors | Optimized imidazole compounds (10, 11, 12) | Inhibit BlaR1 phosphorylation | Compound 12 shows broad efficacy across strains [5] |
| Anti-Phospho Antibodies | Anti-phosphotyrosine, anti-phosphoserine | Detection of BlaR1 phosphorylation states | Anti-phosphothreonine shows no detection [5] |
| Structural Biology Tools | Cryo-EM optimized BlaR1 constructs | Elucidate inhibition mechanisms | F284A mutation prevents autocleavage [3] |
| AI-Designed Compounds | MIT-generated DN1 compound | Novel chemotypes for BlaR1 inhibition | Membrane-targeting mechanism [64] |
The strategic inhibition of BlaR1 represents a promising approach for resensitizing MRSA to β-lactam antibiotics, potentially extending the clinical lifespan of these essential therapeutics. The experimental frameworks outlined herein provide comprehensive methodologies for evaluating BlaR1 inhibitors, monitoring resistance evolution, and implementing combination strategies to mitigate resistance development. By integrating structural insights with functional assays and proactive resistance monitoring, researchers can advance BlaR1-targeted therapies with reduced susceptibility to evolutionary bypass. The continued refinement of these approaches, particularly through structure-guided design and AI-enabled compound generation, offers significant potential for overcoming one of the most challenging aspects of antimicrobial drug development.
Bench to Bedside: Validating BlaR1 Inhibition Against Alternative MRSA Strategies
This application note provides a detailed framework for evaluating the in vitro efficacy of BlaR sensor inhibitors and their synergistic potential with β-lactam antibiotics against methicillin-resistant Staphylococcus aureus (MRSA). The primary goal of these methodologies is to resensitize MRSA to standard antibiotics by disrupting the BlaR1/MecI regulatory system, a key pathway conferring resistance. The protocols outline the use of checkerboard assays and time-kill kinetics to quantitatively measure reductions in Minimum Inhibitory Concentrations (MICs) and synergistic interactions. A novel gene-silencing approach using exosome-delivered siRNA is also detailed, demonstrating a modern strategy to reverse antibiotic resistance at the genetic level. These standardized procedures are designed for researchers and drug development professionals aiming to develop novel therapeutic combinations to combat the global MRSA threat.
The BlaR1 sensor, a transmembrane protein, initiates a critical resistance signaling cascade in MRSA upon perceiving β-lactam antibiotics. This signal leads to the proteolytic cleavage of the MecI repressor, subsequently inducing the expression of the mecA gene [65]. The mecA gene encodes penicillin-binding protein 2a (PBP2a), which has a low affinity for β-lactam antibiotics, allowing for cell wall synthesis to proceed even in the presence of these drugs [66]. Inhibiting the BlaR1 sensor disrupts this signaling pathway, preventing mecA expression and thereby resensitizing MRSA to β-lactam antibiotics [66].
The diagram below illustrates this key resistance pathway and the proposed inhibition strategy.
The following tables summarize key quantitative data from seminal studies investigating resistance reversal strategies against MRSA.
Table 1: Efficacy of Gene Silencing on MRSA Resensitization [66]
| Parameter | Experimental Value | Experimental Outcome |
|---|---|---|
| siRNA Target | mecA gene | Silences PBP2a expression |
| Delivery System | Exosomes (siMecA-Exos) | Facilitates cellular uptake of siRNA |
| PBP2a Reduction | Significant decrease | Restores β-lactam sensitivity |
| In Vivo Survival | 70% survival rate | Lethal MRSA infection model with methicillin treatment |
Table 2: Synergistic Cefiderocol Combinations Against XDR A. baumannii [67] Cefiderocol is a siderophore cephalosporin, a type of β-lactam antibiotic. Its synergistic profiles are informative for combination studies.
| Antibiotic Combination | Strains Tested | Synergy Rate | Key Finding |
|---|---|---|---|
| Cefiderocol + Ceftazidime/Avibactam | XDR/PDR A. baumannii | 100% | Universal, strong synergy |
| Cefiderocol + Sulbactam/Durlobactam | XDR/PDR A. baumannii | 95.2% | Near-universal synergy |
| Cefiderocol + Amikacin | XDR/PDR A. baumannii | >50% | Effective additive/synergistic effect |
Experimental Protocols
Checkerboard Assay for Synergy Screening
This protocol is used to quantitatively measure the synergistic interaction between a BlaR1 inhibitor and a β-lactam antibiotic against MRSA isolates by calculating the Fractional Inhibitory Concentration Index (FICI) [67].
Procedure:
- Preparation of Agents: Prepare stock solutions of the β-lactam antibiotic and the BlaR1 inhibitor in appropriate solvents (e.g., sterile water, DMSO).
- Broth Microdilution Setup:
- Dispense cation-adjusted Mueller-Hinton broth (CAMHB) into a 96-well microtiter plate.
- Serially dilute the β-lactam antibiotic along the x-axis (e.g., 2-fold dilutions from 128 µg/mL to 0.25 µg/mL).
- Serially dilute the BlaR1 inhibitor along the y-axis.
- The final volume in each well before inoculation should be 50 µL.
- Inoculation: Prepare a bacterial suspension of the MRSA test strain equivalent to a 0.5 McFarland standard (~1.5 x 10^8 CFU/mL). Dilute this suspension to achieve a final inoculum of approximately 5 x 10^5 CFU/mL in CAMHB. Add 50 µL of this suspension to each well, bringing the total volume to 100 µL. Include growth control (bacteria, no drug) and sterility control (media only) wells.
- Incubation: Incub the plate at 37°C for 18-24 hours.
- MIC Determination: The MIC of each agent alone and in combination is defined as the lowest concentration that prevents visible growth.
- FICI Calculation:
- Calculate the FIC of each agent: FICAntibiotic = (MIC of antibiotic in combination) / (MIC of antibiotic alone). FICInhibitor = (MIC of inhibitor in combination) / (MIC of inhibitor alone).
- Calculate the FICI: FICI = FICAntibiotic + FICInhibitor.
- Interpretation: FICI ≤ 0.5 indicates synergy; 0.5 < FICI ≤ 4.0 indicates no interaction (additivity/indifference); FICI > 4.0 indicates antagonism [67].
Time-Kill Kinetics Assay
This protocol evaluates the bactericidal activity and the rate of killing achieved by the combination of a BlaR1 inhibitor and a β-lactam antibiotic over time, providing dynamic information that static MIC tests cannot [68].
Procedure:
- Setup: Prepare flasks containing CAMHB with the following treatments:
- The β-lactam antibiotic at 0.5x or 1x its MIC.
- The BlaR1 inhibitor at a sub-inhibitory concentration.
- The combination of the β-lactam and the inhibitor at the same concentrations used alone.
- A growth control (no agents).
- Inoculation: Inoculate each flask with the MRSA test strain to a final concentration of ~5 x 10^5 CFU/mL.
- Sampling and Plating: Incubate the flasks at 37°C with shaking. At predetermined time points (e.g., 0, 2, 4, 8, and 24 hours), remove a 100 µL sample from each flask. Perform serial 10-fold dilutions in sterile saline and plate 100 µL of each dilution onto Mueller-Hinton Agar (MHA) plates.
- Enumeration and Analysis: After incubating the plates for 18-24 hours at 37°C, count the colony-forming units (CFU/mL) on plates with 30-300 colonies. Plot the log10 CFU/mL versus time for each treatment.
- Synergy Definition: Synergy is defined as a ≥ 2-log10 decrease in CFU/mL by the combination compared to the most active single agent at a specific time point. Bactericidal activity is defined as a ≥ 3-log10 reduction in CFU/mL from the initial inoculum [68].
Exosome-Mediated siRNA Delivery for mecA Silencing
This protocol describes a novel method to resensitize MRSA by silencing the mecA gene using siRNA delivered via exosomes, effectively turning MRSA into a methicillin-sensitive strain [66].
Procedure:
- siRNA Design and Complexation:
- Design a specific siRNA (e.g., siMecA) targeting the mecA gene mRNA sequence.
- Complex the siMecA with the human Argonaute 2 (AGO2) protein to form the siMecA-AGO2 complex, which is necessary for translational suppression in bacterial cells.
- Exosome Loading and Purification:
- Load the siMecA-AGO2 complex into exosomes, either by co-incubation with purified exosomes or by transfecting producer cells (e.g., HEK293T) with the siRNA and collecting the exosomes they naturally secrete.
- Isolate and purify the loaded exosomes (siMecA-Exos) from the cell culture supernatant via ultracentrifugation or commercial kits.
- In Vitro Treatment:
- Grow the target MRSA strain to mid-log phase.
- Incubate the bacteria with the siMecA-Exos preparation for a defined period (e.g., 4-6 hours).
- Efficacy Assessment:
- Western Blot: Assess the knockdown efficiency by measuring PBP2a protein levels using Western blot analysis.
- MIC Test: Perform a standard broth microdilution test with methicillin or oxacillin to confirm the resensitization. A significant reduction (e.g., 4 to 8-fold) in MIC indicates successful reversal of resistance.
The workflow for this gene-silencing approach is illustrated below.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for BlaR1 Inhibitor and Synergy Studies
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing (AST) | CLSI-compliant; for broth microdilution [67]. |
| Iron-Depleted CAMHB | Specialized medium for testing siderophore-antibiotics like cefiderocol | Essential for proper functionality [67]. |
| 96-Well Microtiter Plates | Platform for performing high-throughput checkerboard assays | Flat-bottom, sterile, non-treated polystyrene. |
| Beta-Lactam Antibiotics | Reference drugs for combination studies with novel inhibitors | Methicillin, oxacillin, cefoxitin, cefiderocol [67] [66]. |
| siMecA and AGO2 Protein | Key molecules for gene-silencing-based resistance reversal | Designed to target mecA mRNA; complexed with AGO2 for bacterial delivery [66]. |
| Exosome Isolation Kits | For purifying exosomes used as delivery vehicles for siRNA | Ultracentrifugation or commercial kit-based methods [66]. |
| MRSA Control Strains | Essential quality control for ensuring assay validity | Includes well-characterized ATCC strains and clinical isolates. |
The rise of methicillin-resistant Staphylococcus aureus (MRSA) represents a critical global health challenge, necessitating the development of novel therapeutic strategies. A key mechanism of resistance in MRSA is the expression of penicillin-binding protein 2a (PBP2a), which is encoded by the mecA gene. PBP2a exhibits low affinity for β-lactam antibiotics, allowing bacterial cell wall synthesis to proceed despite antibiotic pressure [28]. The BlaR sensor plays a crucial role in regulating this resistance mechanism. In the context of developing BlaR sensor inhibitors, in vivo validation using murine models is an indispensable step in the preclinical drug development pipeline. This document provides detailed application notes and protocols for evaluating the efficacy of BlaR sensor inhibitors in murine models of MRSA infection, providing a framework for researchers aiming to resensitize MRSA to β-lactam antibiotics.
Murine models are a cornerstone of infectious disease research due to their physiological similarities to humans, affordability, and ease of handling. For MRSA research, these models provide a controlled system to study pathogenesis, host immune responses, and therapeutic efficacy before advancing to clinical trials [69]. The selection of an appropriate murine model is paramount and depends on the specific research question, whether it pertains to systemic infection, localized wound biofilm, or other infection types.
Key Advantages of Murine Models:
- Genetic Tractability: Mouse genes can be manipulated to create transgenic or humanized strains, allowing for the study of specific host-pathogen interactions [69].
- Accessible Tissue Sampling: Their size permits the collection of tissue sections for detailed histopathological examination [69].
- Cost-Effectiveness and Handling: Mice are affordable and easier to house and handle compared to larger animal models, facilitating robust sample sizes in experiments [69].
Established Murine Models for MRSA Infection
Systemic MRSA Infection Model
Systemic (bloodstream) infection models are crucial for evaluating the efficacy of novel compounds against disseminated MRSA, a condition associated with high mortality rates.
- Animal Model: Immunocompetent inbred mouse strains (e.g., BALB/c) are commonly used. The model can be adapted for immunocompromised studies if required.
- Pathogen Strain: MRSA ATCC 33592 is a commonly used multidrug-resistant strain for in vivo validation [70].
- Inoculum Preparation and Infection: MRSA is cultured to mid-log phase, harvested, and washed. Mice are inoculated via intravenous injection (e.g., lateral tail vein) with a defined bacterial load (e.g., ( 1 \times 10^7 ) to ( 5 \times 10^7 ) CFU) in a small volume of saline [70].
- Key Efficacy Endpoints:
- Survival Rate: Mice are monitored for mortality over a predefined period (e.g., 7-14 days).
- Bacterial Burden: At designated time points post-infection, animals are euthanized, and target organs (e.g., kidneys, spleen) are harvested, homogenized, and plated for quantitative CFU enumeration.
- Clinical Scoring: Animals are assessed for signs of illness (e.g., lethargy, piloerection, weight loss).
Recent Validation: A study validating rifabutin-loaded liposomes demonstrated the utility of this model. In a high-infection systemic model, the group treated with the liposomal formulation achieved a 100% survival rate, outperforming free rifabutin and the gold standard vancomycin (40 mg/kg). Furthermore, the rifabutin formulations resulted in lower bacterial burden levels in organs compared to vancomycin, despite using a lower dose (20 mg/kg) [70].
Partial-Thickness Wound Biofilm Model
Biofilms are a significant factor in chronic, non-healing wounds and are notoriously resistant to antimicrobials. This model specifically tests the ability of BlaR inhibitors to penetrate and act within a biofilm matrix.
- Animal Model: Hairless SKH1 mice are preferred to expedite wounding without hair removal and to maintain dressings more easily. Transient neutropenia can be induced with cyclophosphamide (150 mg/kg IP) 4 days prior to facilitate a robust infection [71].
- Wounding and Inoculation: After anesthesia, a partial-thickness wound is created on the dorsum. The wound is then inoculated with a high bacterial load (e.g., ( 2 \times 10^7 ) CFU of MRSA) and covered with a moistened bandage to maintain a wound environment conducive to biofilm formation [71].
- Key Efficacy Endpoints:
- Quantitative Microbiology: Wound biopsy samples are processed and plated to determine the tissue bioburden (CFU/g of tissue) after treatment.
- Histological and Microscopic Analysis: Samples are fixed, sectioned, and stained (e.g., Gram stain, H&E) to visualize biofilm structure and immune cell infiltration. Scanning Electron Microscopy (SEM) can further characterize the biofilm morphology [71].
Model Characterization: In this model, a dense MRSA biofilm community was observed to develop on the wound surface within 24 hours post-inoculation. The geometric mean MRSA bioburden increased from ( 5 \times 10^9 ) CFU/g tissue at 4 hours to ( 2 \times 10^{10} ) CFU/g at 24 hours, remaining stable thereafter. This established biofilm presents a more therapeutically challenging target, as demonstrated by the reduced efficacy of common topical antibiotics like mupirocin and bacitracin when treatment was initiated at 24 hours versus 4 hours [71].
Table 1: Key Murine Models for In Vivo MRSA Efficacy Studies
| Model Type | Mouse Strain | MRSA Strain | Inoculation Route & Dose | Primary Endpoints | Key Characteristics |
|---|---|---|---|---|---|
| Systemic Infection | BALB/c, C3H/HeJ | ATCC 33592, USA300 | Intravenous (IV); ( 1 \times 10^7 ) - ( 5 \times 10^7 ) CFU | Survival, Bacterial burden in organs (CFU/g) | Models bloodstream infection; assesses systemic efficacy. |
| Wound Biofilm | Hairless SKH1 | ATCC 33592 | Topical to wound; ( 2 \times 10^7 ) CFU | Bacterial bioburden in wound (CFU/g), Histology, SEM | Recapitulates chronic wound biofilms; tests penetration and biofilm efficacy. |
Application Note: Evaluating BlaR Sensor Inhibitors
Conceptual Workflow and Rationale
The following diagram illustrates the strategic rationale for using BlaR sensor inhibitors to resensitize MRSA to β-lactam antibiotics, and the subsequent in vivo validation workflow.
Experimental Design for Combination Therapy
BlaR sensor inhibitors are not typically bactericidal on their own but function as potentiators. Therefore, they must be evaluated in combination with a β-lactam antibiotic.
Test Groups: A well-designed study should include the following groups for any given model:
- Untreated Control: Infected but receiving only vehicle.
- β-lactam Monotherapy: e.g., Oxacillin or Meropenem.
- BlaR Inhibitor Monotherapy.
- Combination Therapy: BlaR Inhibitor + β-lactam antibiotic.
- Standard of Care Control: e.g., Vancomycin.
Dosing Regimen: Treatment should initiate after infection is established. For systemic models, this can be 1-2 hours post-infection. For biofilm models, a delayed start (e.g., 24 hours post-inoculation) is critical to assess efficacy against a mature biofilm [71]. Dosing should continue for a predefined period (e.g., 2-4 days, twice daily).
Validated Approach: This strategy has been successfully demonstrated. A recent study using a benzimidazole-derived boronate BlaR inhibitor (Compound 4) showed it covalently binds BlaR's active-site serine. This compound potentiated the activity of oxacillin and meropenem against MRSA by 16- to 4,096-fold in vitro. Furthermore, the combination of this BlaR inhibitor with oxacillin or meropenem showed significant efficacy in infected mice, validating the in vivo approach [15].
Protocol: Efficacy Testing in a Systemic MRSA Model
Objective: To evaluate the efficacy of a BlaR sensor inhibitor in combination with a β-lactam antibiotic in a murine systemic MRSA infection model.
Materials:
- Animals: Female BALB/c mice, 6-8 weeks old.
- Bacterial Strain: MRSA ATCC 33592.
- Test Articles: BlaR inhibitor (BRI), β-lactam antibiotic (e.g., Oxacillin), Vancomycin.
- Equipment: Laminar flow hood, incubator, microcentrifuge, colony counter, sterile surgical instruments.
Procedure:
- MRSA Inoculum Preparation:
- Grow MRSA to mid-log phase in Mueller-Hinton broth.
- Centrifuge, wash, and resuspend in PBS.
- Adjust optical density to achieve a target concentration of ~( 5 \times 10^7 ) CFU/mL. Verify concentration by serial dilution and plating.
Infection:
- Restrain mice in a suitable holder and gently warm the tail to dilate the veins.
- Disinfect the tail with 70% ethanol.
- Slowly inject 200 µL of the bacterial suspension (( ~1 \times 10^7 ) CFU) into the lateral tail vein using a 1 mL syringe with a 29-gauge needle.
Treatment:
- Randomly assign infected mice into the test groups (n=6-10 per group).
- Begin treatment 1-hour post-infection.
- Administer compounds via intraperitoneal (IP) or subcutaneous (SC) injection at predetermined doses (e.g., BRI at 20 mg/kg, Oxacillin at 50 mg/kg, combination therapy) twice daily for 4 days.
- Monitor mice twice daily for mortality and clinical signs.
Endpoint Analysis:
- Survival: Monitor for 7-14 days, recording survival rates.
- Bacterial Burden: Euthanize a subset of mice at 24 or 48 hours post-infection. Aseptically remove kidneys and spleen. Homogenize organs in 1 mL of PBS. Perform serial dilutions and plate on Mannitol Salt Agar. Incubate plates at 37°C for 24 hours and count CFUs. Report results as Log₁₀ CFU per gram of tissue.
Data Interpretation: A successful BlaR inhibitor will show a significant reduction in bacterial burden and an increase in survival rate in the combination group compared to the β-lactam monotherapy and untreated control groups. The results should demonstrate a statistically significant restoration of the β-lactam's efficacy.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Murine MRSA Efficacy Studies
| Item | Function / Application | Example / Specification |
|---|---|---|
| MRSA Strain ATCC 33592 | A standard, well-characterized multidrug-resistant strain for in vivo validation of anti-MRSA therapeutics. | Methicillin-resistant Staphylococcus aureus, genome sequenced. |
| BlaR Sensor Inhibitor | Investigational compound that blocks BlaR signaling, halting PBP2a production and resensitizing MRSA to β-lactams. | e.g., Benzimidazole-based boronate (Compound 4) [15]. |
| β-lactam Antibiotic | Partner antibiotic whose efficacy is being restored. Used in combination with the BlaR inhibitor. | Oxacillin, Meropenem, etc. |
| Hairless SKH1 Mice | Mouse strain ideal for wound biofilm studies; eliminates need for hair removal and facilitates dressing retention. | Crl:SKH1-Hr(^{hr}) [71]. |
| Inbred BALB/c Mice | Common immunocompetent mouse strain for systemic infection models due to well-defined genetics and immune response. | BALB/cAnNCrl [69]. |
| Mueller-Hinton Broth | Standardized growth medium for the cultivation of Staphylococcus aureus and for MIC determination. | Cation-adjusted Mueller-Hinton Broth (CAMHB). |
| Cyclophosphamide | Immunosuppressive agent used to induce transient neutropenia in mice, enabling a more robust infection in wound models. | Single intraperitoneal dose of 150 mg/kg, 4 days pre-study [71]. |
Data Analysis and Reporting
All quantitative data, particularly bacterial burdens, should be presented as geometric means or medians. Statistical analysis (e.g., ANOVA with post-hoc tests for bacterial burden, Log-rank test for survival curves) is essential to demonstrate the significance of the findings. The fold potentiation of the β-lactam antibiotic's activity by the BlaR inhibitor in vivo can be derived from the difference in log₁₀ CFU/g between the monotherapy and combination groups.
Table 3: Example Data Structure for Reporting In Vivo Efficacy
| Experimental Group | Survival at 7 Days (%) | Mean Bacterial Burden in Kidneys (Log₁₀ CFU/g ± SEM) | Statistical Significance (vs. β-lactam monotherapy) |
|---|---|---|---|
| Untreated Control | 0 | 8.5 ± 0.3 | - |
| Oxacillin (50 mg/kg) | 20 | 7.8 ± 0.4 | - |
| BRI (20 mg/kg) | 0 | 8.3 ± 0.2 | p > 0.05 |
| BRI + Oxacillin | 100 | 3.2 ± 0.5 | p < 0.001 |
| Vancomycin (40 mg/kg) | 100 | 2.8 ± 0.3 | p < 0.001 (vs. Untreated) |
Comparative Analysis with PBP2a-Targeting Strategies and Allosteric Inhibitors
Methicillin-resistant Staphylococcus aureus (MRSA) represents a critical global health threat, accounting for hundreds of thousands of infections and tens of thousands of deaths annually according to recent epidemiological data [18]. The fundamental mechanism underlying MRSA's resistance to β-lactam antibiotics involves two key components: the sensor-transducer protein BlaR1 and the resistance determinant penicillin-binding protein 2a (PBP2a). While BlaR1 detects antibiotic presence and initiates signal transduction leading to resistance expression, PBP2a maintains bacterial cell wall synthesis even in the presence of β-lactam antibiotics due to its sheltered active site that exhibits markedly reduced affinity for these drugs [28] [72]. This application note provides a comparative analysis of therapeutic strategies targeting these systems, with particular emphasis on allosteric inhibition mechanisms, quantitative efficacy data, and standardized experimental protocols for evaluating novel compounds.
The clinical significance of MRSA infections stems from the bacterium's resistance to multiple antibiotic classes and its ability to cause life-threatening conditions. According to recent surveillance data, MRSA strains account for approximately 32.2% of Gram-positive bacterial isolates in clinical settings, highlighting the persistent challenge they pose to healthcare systems worldwide [73]. The escalating resistance to last-line treatments like vancomycin further underscores the urgent need for innovative therapeutic approaches that can resensitize MRSA to conventional antibiotics [73].
Molecular Mechanisms of MRSA Resistance
BlaR1-Mediated Signal Transduction and Resistance Induction
The integral membrane protein BlaR1 functions as both a β-lactam sensor and signal transducer. Upon exposure to β-lactam antibiotics, the sensor domain of BlaR1 becomes acylated, initiating an intracellular signaling cascade. Recent research has revealed that this process involves phosphorylation of specific serine and tyrosine residues within BlaR1's cytoplasmic domain, an event critical for the induction of antibiotic resistance [5]. The phosphorylation activates the cytoplasmic zinc protease domain of BlaR1, which subsequently degrades the gene repressor BlaI. This proteolytic degradation derepresses the transcription of resistance genes, including those encoding BlaR1 itself and the resistance determinants β-lactamase and PBP2a [5] [1].
The induction process is notably reversible; once antibiotic challenge is withdrawn, the system resets through specific fragmentation of BlaR1. Research has identified two primary proteolytic sites: one in the cytoplasmic domain and another in the sensor domain, the latter resulting in shedding of the extracellular domain into the medium [1]. This fragmentation mechanism facilitates recovery from induction once the antibiotic pressure subsides, representing a sophisticated regulatory system that allows MRSA to adapt dynamically to environmental threats.
PBP2a Structure and Allosteric Regulation
PBP2a, encoded by the acquired mecA gene, possesses a unique architectural feature: an allosteric binding site located approximately 60 Å from the active site [74] [73]. In the absence of allosteric triggers, the active site remains in a closed conformation, guarded by surrounding protein loops (specifically the α2-α3 and β3-β4 loops) that physically block β-lactam antibiotics from effective binding [74] [28]. This structural arrangement explains PBP2a's markedly reduced affinity for most β-lactam antibiotics.
The allosteric mechanism is triggered when specific ligands—including natural peptidoglycan substrates or synthetic inhibitors—bind to the allosteric site. This binding induces conformational changes that propagate through the protein structure, ultimately resulting in opening of the active site. Computational simulations using molecular dynamics have revealed that allosteric binding stabilizes the allosteric domain while simultaneously enhancing the dynamics of the catalytic domain, particularly the loops guarding the active site [74]. This opening allows a second molecule (either substrate or antibiotic) to access and bind to the now-accessible active site, completing the inhibition process in the case of effective antibiotics.
Table 1: Key Genetic Determinants of MRSA β-Lactam Resistance
| Genetic Element | Protein Encoded | Function | Role in Resistance |
|---|---|---|---|
| mecA | PBP2a | Cell wall synthesis with low β-lactam affinity | Primary resistance determinant; bypasses antibiotic inhibition |
| blaR1 | BlaR1 | β-lactam sensor/signal transducer | Initiates resistance induction via signal transduction |
| mecI/mecR1 or blaI/blaR1 | MecI/MecR1 or BlaI/BlaR1 | Regulatory genes for PBP2a expression | Controls expression levels of resistance machinery |
| SCCmec | Mobile genetic element | Carrier of mecA and regulatory genes | Horizontal transfer of resistance genes |
Comparative Analysis of Targeting Strategies
Allosteric Inhibitors of PBP2a
Ceftaroline: The Pioneering Allosteric Trigger
Ceftaroline, a fifth-generation cephalosporin approved by the FDA in 2010, represents the first commercialized antibiotic that effectively inhibits PBP2a through a dual-binding mechanism [74] [73]. Its mode of action involves two distinct molecules: the first ceftaroline molecule (CFT1) binds non-covalently to the allosteric site, triggering conformational changes that open the active site. This opening allows a second ceftaroline molecule (CFT2) to covalently acylate the active site serine residue (Ser403), effectively inhibiting PBP2a's transpeptidase activity [74]. Molecular dynamics simulations have elucidated that CFT1 binding stabilizes the allosteric domain while increasing flexibility in the catalytic domain, particularly in the α2-α3 and β3-β4 loops that guard the active site [74].
The efficacy of ceftaroline is demonstrated by its low minimum inhibitory concentration (MIC) against various MRSA strains, typically ranging from 0.25 μg/mL to 1 μg/mL [73]. However, resistance has emerged through mutations at both active and allosteric sites. High-level resistance (MIC > 32 μg/mL) is associated with active site mutations (Y446N and E447K), while moderate resistance (MIC 2-4 μg/mL) correlates with allosteric site mutations (N146K and E150K) [73]. This mutation pattern underscores the clinical importance of the allosteric mechanism and highlights the need for next-generation inhibitors targeting this site.
Quinazolinones: Synergistic Allosteric Inhibitors
The quinazolinones represent a novel class of orally bioavailable anti-MRSA agents that specifically target the PBP2a allosteric site [75]. Compound 2, a lead quinazolinone, demonstrates potent activity against MRSA with MIC values ranging from 0.03 to 1 μg/mL across various strains [75]. Notably, quinazolinones exhibit strong synergy with β-lactam antibiotics such as piperacillin and oxacillin, with fractional inhibitory concentration (FIC) indices of 0.5 indicating marginal synergy in checkerboard assays [75].
The proposed mechanism involves quinazolinone binding to the allosteric site, which triggers the allosteric response and opens the active site, allowing concomitant β-lactam antibiotics to inhibit PBP2a. This synergistic effect has demonstrated bactericidal activity in time-kill assays and efficacy in mouse neutropenic thigh infection models [75]. The triple combination of a quinazolinone with piperacillin-tazobactam showed particularly promising results, with tazobactam inhibiting β-lactamase activity and protecting piperacillin from hydrolysis, while the quinazolinone sensitized PBP2a to piperacillin inhibition [75].
Novel Nucleoside Inhibitors
Recent advances have identified novel nucleoside derivatives as promising allosteric inhibitors of PBP2a. Through virtual screening of a nucleoside compound library (TMME) targeting the PBP2a allosteric site, researchers identified and optimized compound 2-8e, which demonstrates significant anti-MRSA activity with an MIC of 16 μg/mL [73] [76]. Time-kill curve analysis confirmed that compound 2-8e effectively inhibits bacterial growth, and morphological studies revealed disruption of bacterial cell wall integrity following treatment [76].
A particularly interesting finding is the compound's synergistic effect with oxacillin at low concentrations, though antagonism was observed at higher concentrations [76]. This nucleoside inhibitor also demonstrates a lower propensity for resistance development compared to cephalosporins and shows no cytotoxicity against normal human intestinal epithelial cells (HIEC) and brain microvascular endothelial cells at concentrations significantly above its MIC [76]. These characteristics highlight the potential of nucleoside-based allosteric inhibitors as promising candidates for further development.
Table 2: Comparative Analysis of PBP2a Allosteric Inhibitors
| Inhibitor Class | Representative Compound | MIC Range (μg/mL) | Synergy with β-Lactams (FIC Index) | Key Advantages | Resistance Concerns |
|---|---|---|---|---|---|
| Cephalosporins | Ceftaroline | 0.25 - 1 [73] | N/A (direct inhibitor) | Established clinical use; dual-binding mechanism | Emerging resistance via active site (Y446N, E447K) and allosteric site (N146K, E150K) mutations [73] |
| Quinazolinones | Compound 2 | 0.03 - 1 [75] | 0.5 (synergistic with piperacillin, oxacillin) [75] | Oral bioavailability; in vivo efficacy; synergistic combinations | Limited standalone resistance data; primarily studied in combinations |
| Nucleosides | Compound 2-8e | 16 [76] | Concentration-dependent synergy with oxacillin [76] | Low cytotoxicity; novel chemical scaffold; low resistance propensity | Higher MIC than conventional antibiotics; requires optimization |
| Imidazole-based kinase inhibitors | Compound 1, 10, 11, 12 | >64 (alone); significantly reduces oxacillin MIC [5] | Reduces oxacillin MIC 4-64 fold [5] | Targets BlaR1 phosphorylation; reverses resistance phenotype | Early research stage; mechanism distinct from direct PBP2a inhibition |
BlaR1-Targeted Strategies
Emerging approaches focus on inhibiting the BlaR1-mediated signaling pathway that regulates resistance expression. Research has demonstrated that BlaR1 undergoes phosphorylation on specific serine and tyrosine residues upon β-lactam exposure, and that this phosphorylation event is critical for induction of the resistance response [5]. Synthetic protein kinase inhibitors, particularly optimized imidazole analogues (compounds 10, 11, and 12), have been shown to inhibit BlaR1 phosphorylation and reverse the methicillin-resistant phenotype, restoring susceptibility to β-lactam antibiotics [5].
In experimental models, these inhibitors reduced phosphorylation of BlaR1 by 70-90% and lowered the MIC of oxacillin by 4 to 64-fold across multiple MRSA strains [5]. For instance, in strain MRSA252, compound 10 reduced the oxacillin MIC from 256 μg/mL to 2 μg/mL, while in strain NRS70, compounds 11 and 12 reduced the oxacillin MIC from 32 μg/mL to 0.5 μg/mL [5]. This approach represents a paradigm shift from targeting the resistance determinant itself to preventing the induction of resistance, potentially extending the utility of existing β-lactam antibiotics.
Experimental Protocols and Methodologies
Protocol 1: Evaluation of Allosteric Inhibitor Efficacy
4.1.1 Broth Microdilution MIC Determination Materials Required: Cation-adjusted Mueller-Hinton II broth, sterile 96-well polypropylene microplates, bacterial inoculum suspension equivalent to 0.5 McFarland standard, doubling dilutions of test compound, oxacillin as control antibiotic. Procedure:
- Prepare serial twofold dilutions of the test compound in Mueller-Hinton II broth across the microplate wells.
- Standardize the bacterial inoculum to approximately 5 × 10^5 CFU/mL in each well.
- Include growth control (inoculum without antibiotic) and sterility control (medium only) wells.
- Incubate plates at 35°C ± 2°C for 16-20 hours.
- Determine MIC as the lowest concentration completely inhibiting visible growth.
- For synergy studies, incorporate fixed subinhibitory concentrations of companion antibiotics [5] [75].
4.1.2 Checkerboard Synergy Assay Materials Required: As above, with two antimicrobial agents for combination testing. Procedure:
- Prepare serial dilutions of Drug A along the x-axis and Drug B along the y-axis.
- Calculate the Fractional Inhibitory Concentration (FIC) index using the formula: FIC index = (MIC of Drug A in combination/MIC of Drug A alone) + (MIC of Drug B in combination/MIC of Drug B alone).
- Interpret results: FIC index ≤ 0.5 indicates synergy; >0.5 to 4 indicates indifference; >4 indicates antagonism [75].
Protocol 2: Time-Kill Kinetics Assay
4.2.1 Bactericidal Activity Assessment Materials Required: Cation-adjusted Mueller-Hinton II broth, test compounds at relevant concentrations, sterile plastic tubes, viable count methodology materials. Procedure:
- Prepare bacterial suspensions approximating 5 × 10^5 CFU/mL in tubes containing antimicrobial agents at specified concentrations.
- Include growth control tubes without antimicrobial agents.
- Incubate at 35°C ± 2°C with shaking.
- Remove aliquots at 0, 4, 8, and 24 hours for viable counting.
- Serially dilute aliquots in sterile saline and plate on Mueller-Hinton agar.
- Count colonies after 18-24 hours incubation and calculate CFU/mL.
- Define bactericidal activity as ≥3-log10 decrease in CFU/mL compared to initial inoculum [76] [75].
Protocol 3: Phosphorylation Inhibition Assay
4.3.1 Western Blot Analysis of BlaR1 Phosphorylation Materials Required: S. aureus cultures, induction agents (e.g., CBAP at 10 μg/mL), protein kinase inhibitors, lysis buffer (100 mM sodium phosphate, pH 7.5, 50 mM NaHCO3, protease inhibitor cocktail, 1 mM EDTA, 20 mM MgCl2, lysostaphin), SDS-PAGE equipment, anti-phosphotyrosine and anti-phosphoserine antibodies. Procedure:
- Grow S. aureus cultures to exponential phase (A625 ≈ 0.8).
- Divide cultures and treat with: (a) no inducer, (b) CBAP inducer alone, (c) CBAP + varying concentrations of kinase inhibitors.
- Incubate for specified durations (15 min to 3 h).
- Harvest cells by centrifugation and prepare whole-cell extracts.
- Quantify total protein using BCA assay.
- Separate 60-80 μg total protein by Tris-glycine SDS-PAGE.
- Transfer to membranes and probe with anti-phosphotyrosine and anti-phosphoserine antibodies.
- Quantify band intensity to determine percentage phosphorylation inhibition [5].
Signaling Pathway Visualization
Diagram 1: BlaR1 Signaling Pathway and Inhibition Mechanism. This diagram illustrates the signal transduction pathway initiated by β-lactam binding to BlaR1, culminating in expression of resistance determinants. The critical phosphorylation step and its inhibition by kinase inhibitors are highlighted.
Diagram 2: PBP2a Allosteric Inhibition Mechanism. This diagram illustrates the allosteric regulation of PBP2a and the mechanism by which allosteric inhibitors restore β-lactam antibiotic efficacy against MRSA.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MRSA Resistance Studies
| Reagent/Chemical | Function/Application | Example Usage | Key Considerations |
|---|---|---|---|
| CBAP (2-(2'-carboxyphenyl)-benzoyl-6-aminopenicillanate) | Potent penicillin-based inducer of bla operon | Induction of BlaR1 signaling at 10 μg/mL [5] | More effective inducer than natural penicillins; use at 6.4-fold below MIC for standardization |
| Anti-phosphotyrosine & anti-phosphoserine antibodies | Detection of BlaR1 phosphorylation | Western blot analysis of BlaR1 phosphorylation status [5] | Critical for validating kinase inhibitor efficacy; requires specific extraction protocols |
| Protein kinase inhibitor library | Screening for BlaR1 phosphorylation inhibitors | Identification of compound 1 as lead inhibitor [5] | Includes 80 known compounds; screen at 0.7 and 7 μg/mL concentrations |
| Quinazolinone compound 2 | Allosteric PBP2a inhibitor | Synergy studies with β-lactams; MIC 0.25 μg/mL against NRS70 [75] | Oral bioavailability; large volume of distribution (3.58 L/kg); terminal half-life 6.5 h |
| Nucleoside compound 2-8e | Novel allosteric PBP2a inhibitor | Anti-MRSA activity studies; MIC 16 μg/mL [76] | Low cytotoxicity; novel scaffold; synergistic with oxacillin at low concentrations |
| Piperacillin-tazobactam combination | β-lactam/β-lactamase inhibitor combination | Triple therapy with quinazolinones [75] | Tazobactam protects piperacillin from hydrolysis; quinazolinone opens PBP2a active site |
| Lysostaphin | Cell wall digestion for protein extraction | Preparation of S. aureus whole-cell extracts [5] [1] | Essential for efficient bacterial lysis; use at 200 μg/mL in lysis buffer |
The comparative analysis presented in this application note demonstrates that both PBP2a allosteric inhibitors and BlaR1-targeted strategies offer promising avenues for overcoming MRSA resistance. Allosteric PBP2a inhibitors, particularly when used in synergistic combinations, represent a mature approach with demonstrated clinical utility, as evidenced by ceftaroline. Meanwhile, BlaR1 phosphorylation inhibitors offer a novel mechanism that prevents resistance induction rather than combating established resistance mechanisms.
Future research directions should focus on optimizing the chemical scaffolds of nucleoside and quinazolinone inhibitors to improve potency and pharmacokinetic properties. Additionally, combination therapies that simultaneously target both BlaR1 signaling and PBP2a function may provide enhanced efficacy and reduce the emergence of resistance. The experimental protocols and research tools outlined herein provide a standardized framework for evaluating novel compounds and advancing innovative strategies to resensitize MRSA to β-lactam antibiotics, addressing one of the most pressing challenges in antimicrobial therapy.
Positioning BlaR1 Inhibition within the Anti-Virulence Framework
Methicillin-resistant Staphylococcus aureus (MRSA) represents a critical global health challenge, characterized by its resistance to multiple β-lactam antibiotics and association with high mortality rates [28] [77]. A key molecular mechanism underlying this resistance involves the BlaR1 receptor, an integral membrane protein that functions as a β-lactam sensor and signal transducer [1] [5]. Upon detection of β-lactam antibiotics in the bacterial environment, BlaR1 initiates a signaling cascade that ultimately activates expression of resistance determinants, primarily the blaZ-encoded β-lactamase PC1 and the mecA-encoded penicillin-binding protein 2a (PBP2a) [3] [77]. The PBP2a protein exhibits markedly low affinity for β-lactams, allowing peptidoglycan synthesis to continue despite antibiotic presence [28]. This sophisticated sensing and response system makes BlaR1 an attractive target for anti-virulence strategies aimed at resensitizing MRSA to conventional antibiotics rather than directly killing the pathogen [78] [20].
Molecular Mechanisms of BlaR1-Mediated Signaling
Signal Transduction Pathway
The BlaR1-mediated resistance mechanism operates through a precisely regulated molecular pathway. BlaR1 is an integral membrane protein featuring an extracellular β-lactam-sensing domain and a cytoplasmic zinc metalloprotease domain [3]. When β-lactam antibiotics acylate the sensor domain on the bacterial surface, a conformational change occurs that transmits the signal across the membrane [1]. Recent cryo-EM structural analyses reveal that BlaR1 forms a domain-swapped dimer, with the N-terminal zinc metalloprotease domain exhibiting an unusual Nout, Cout topology [3]. This dimerization creates a central cavity lined with phosphatidylglycerol headgroups, suggesting lipid involvement in the signaling process [3].
The signal transduction triggers two critical downstream events: activation of the cytoplasmic metalloprotease domain and phosphorylation of BlaR1 itself. The metalloprotease domain, characterized by H201EXXH and E242XXXD gluzincin signature motifs, becomes activated and cleaves the BlaI repressor protein [3]. Concurrently, BlaR1 undergoes phosphorylation on at least one serine and one tyrosine residue within its cytoplasmic domain, an event that appears essential for full activation of the resistance response [5]. BlaI cleavage derepresses transcription of the bla operon, leading to increased production of β-lactamase and PBP2a, which collectively confer antibiotic resistance [1] [3].
Figure 1: BlaR1-Mediated Resistance Signaling Pathway
Structural Basis of BlaR1 Activation
Structural studies have illuminated the allosteric mechanisms governing BlaR1 activation. The receptor exists as a domain-swapped dimer that stabilizes signaling loops within the protein [3]. A prominent feature is the autocleavage loop (residues 271-289), which undergoes spontaneous cleavage between Ser283 and Phe284 in the zinc metalloprotease active site [3]. β-lactam binding to the extracellular sensor domain competitively displaces a prominent extracellular loop, initiating structural rearrangements that propagate toward the membrane. This triggers a shift in the sensor domain and accompanying conformational changes in the metalloprotease domain that enhance expulsion of autocleaved products from the active site, creating a state permissive for efficient BlaI cleavage [3]. The discovery of these structural dynamics provides crucial insights for targeted inhibition strategies.
Quantitative Assessment of BlaR1 Inhibition Strategies
Synthetic Kinase Inhibitors
Recent research has identified several synthetic compounds that effectively inhibit BlaR1 signaling through disruption of its phosphorylation-dependent activation.
Table 1: Efficacy of Synthetic BlaR1 Kinase Inhibitors in MRSA Strains
| Compound | Chemical Class | MRSA252 MIC Reduction | NRS123 MIC Reduction | NRS70 MIC Reduction | Primary Mechanism |
|---|---|---|---|---|---|
| 10 | Optimized imidazole | 256→2 μg/mL | 16→8 μg/mL | 32→4 μg/mL | Tyrosine phosphorylation inhibition |
| 11 | Optimized imidazole | 256→16 μg/mL | 16→4 μg/mL | 32→0.5 μg/mL | Tyrosine phosphorylation inhibition |
| 12 | Optimized imidazole | 256→4 μg/mL | 16→4 μg/mL | 32→0.5 μg/mL | Tyrosine phosphorylation inhibition |
| Compound 4 | Benzimidazole | Restores oxacillin & meropenem sensitivity in 40 strains | N/A | N/A | Active site binding & signal blockade |
Natural and Nucleic Acid-Based Inhibitors
Alternative inhibition approaches leverage natural compounds and gene-targeting strategies to disrupt BlaR1 function.
Table 2: Natural and Nucleic Acid-Based BlaR1 Inhibitors
| Inhibitor | Source/Type | Binding Affinity | Proposed Mechanism | Experimental Validation |
|---|---|---|---|---|
| Lucidenic acid F | Ganoderma lucidum mushroom | -7.4 kcal/mol | Active site binding | In silico docking (PDB:1XA1) |
| PS-DRz1366 | Phosphorothioate deoxyribozyme | N/A | mecR1 mRNA cleavage | 60-75% reduced blaR1 transcription |
| PS-DRz1694 | Phosphorothioate deoxyribozyme | N/A | blaR1 mRNA cleavage | Enhanced β-lactam susceptibility |
Experimental Protocols for BlaR1 Inhibition Studies
Protocol 1: Evaluation of BlaR1 Kinase Inhibitors
Purpose: To assess the efficacy of synthetic kinase inhibitors in restoring β-lactam sensitivity in MRSA strains.
Materials:
- MRSA strains (e.g., MRSA252, NRS123, NRS70)
- Cation-adjusted Mueller-Hinton II broth
- β-lactam antibiotics (oxacillin, meropenem)
- Kinase inhibitors (compounds 10, 11, 12, or compound 4)
- 96-well microtiter plates
- Microplate spectrophotometer
Procedure:
- Prepare logarithmic-phase MRSA cultures in Mueller-Hinton II broth (adjusted to 5 × 10^5 CFU/mL).
- Dispense bacterial suspension into 96-well plates containing serial dilutions of β-lactam antibiotics.
- Add kinase inhibitors at sub-inhibitory concentrations (0.7-7 μg/mL based on preliminary MIC testing).
- Include controls: growth (no antibiotics), solvent (DMSO), and antibiotic-only.
- Incubate plates at 37°C for 20 hours.
- Measure optical density at 625 nm to determine minimum inhibitory concentrations (MICs).
- Calculate fold-reduction in MIC compared to antibiotic-only controls [5].
Validation:
- For phosphorylation analysis: Perform Western blotting with anti-phosphotyrosine and anti-phosphoserine antibodies on whole-cell extracts from inhibitor-treated cultures [5].
Protocol 2: Molecular Docking for Natural Inhibitor Screening
Purpose: To identify and evaluate potential BlaR1 inhibitors from natural compound libraries.
Materials:
- BlaR1 sensor domain structure (PDB ID: 1XA1)
- Natural compound library (e.g., KNApSAcK Ganoderma lucidum metabolites)
- Molecular docking software (AutoDock Vina, PyRx)
- Visualization software (UCSF ChimeraX, BIOVIA Discovery Studio)
- SwissADME web tool for pharmacokinetic prediction
Procedure:
- Download and prepare BlaR1 target structure: remove water molecules, add polar hydrogens, define grid box around active site.
- Prepare ligand library: obtain 3D structures of natural compounds, perform energy minimization.
- Conduct molecular docking using validated parameters (exhaustiveness = 8, max poses = 10).
- Analyze results: rank compounds by binding affinity (kcal/mol), inspect binding poses.
- Filter hits using SwissADME: assess Lipinski's Rule of Five compliance, pharmacokinetics.
- Predict acute toxicity using GUSAR and QSAR platforms.
- Visualize protein-ligand interactions (hydrogen bonds, hydrophobic contacts) [79].
Validation:
- Select top candidates (e.g., Lucidenic acid F) for in vitro validation using β-lactamase induction assays [79].
Protocol 3: Deoxyribozyme-Mediated Gene Suppression
Purpose: To knock down BlaR1 expression using sequence-specific deoxyribozymes.
Materials:
- Phosphorothioate deoxyribozymes (PS-DRz1366, PS-DRz1694)
- MRSA clinical isolates with varying mecI/blaI genotypes
- Electroporation apparatus
- Trizol reagent for RNA extraction
- RT-PCR system with SYBR Green
- In vitro transcription system
Procedure:
- Design 10-23 deoxyribozymes targeting accessible regions of mecR1 and blaR1 mRNA using RNAstructure 4.6.
- Synthesize deoxyribozymes with phosphorothioate modifications for nuclease resistance.
- Prepare electrocompetent MRSA cells: wash logarithmic-phase cultures with ice-cold 10% glycerol.
- Introduce deoxyribozymes (10 mg/L) via electroporation (25 μF, 900 V, 200 Ω).
- Incubate recovered cultures with sub-MIC β-lactams for induction.
- Extract total RNA and synthesize cDNA for RT-PCR analysis.
- Quantify mecR1 and blaR1 transcript levels using gene-specific primers [20].
Validation:
- Assess blaZ and mecA expression levels to confirm downstream effects.
- Determine antibiotic susceptibility changes post-treatment [20].
Figure 2: BlaR1 Inhibitor Screening Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for BlaR1 Inhibition Research
| Reagent/Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| MRSA Strains | MRSA252 (USA200), NRS123 (MW2), NRS70 (N315) | Model organisms for resistance studies | Varied genetic backgrounds; differential BlaR1 expression |
| Synthetic Inhibitors | Compound 4 (benzimidazole), Compounds 10-12 (imidazoles) | Kinase inhibition; BlaR1 signal disruption | Target tyrosine phosphorylation; restore β-lactam efficacy |
| Natural Compounds | Lucidenic acid F (from Ganoderma lucidum) | BlaR1 active site binding | Binding affinity: -7.4 kcal/mol; favorable ADMET properties |
| Gene Targeting Tools | PS-DRz1366, PS-DRz1694 (phosphorothioate deoxyribozymes) | mRNA cleavage for mecR1/blaR1 knockdown | Enhanced nuclease resistance; specific catalytic activity |
| Structural Biology Resources | BlaR1 sensor domain (PDB:1XA1); Full-length BlaR1 cryo-EM structures | Rational drug design; mechanism studies | Reveal allosteric signaling; domain-swapped dimer architecture |
| Antibiotic Inducers | CBAP, oxacillin, ampicillin, meropenem | Resistance pathway induction | β-lactam sensors; trigger BlaR1 signaling cascade |
BlaR1 inhibition represents a promising anti-virulence strategy that operates within a fundamentally different paradigm compared to traditional bactericidal approaches. By targeting the sensory apparatus that MRSA uses to detect and respond to β-lactam antibiotics, this strategy potentially restores the efficacy of existing antibiotics rather than requiring development of entirely new drug classes. The structural insights from recent cryo-EM studies, combined with the demonstrated efficacy of multiple inhibitor classes across diverse MRSA strains, provide a robust foundation for future therapeutic development [78] [3]. The successful in vivo validation of compound 4 in mouse models represents a particularly significant advancement toward clinical application [78].
Future research directions should focus on optimizing the pharmacokinetic properties of lead compounds, exploring combination therapies that target both BlaR1 and complementary resistance mechanisms, and investigating potential synergies with conventional antibiotics. Additionally, the differential regulation of bla and mec divergons across MRSA strains necessitates carefully tailored approaches based on the genetic background of clinical isolates [77] [20]. As the field progresses, BlaR1 inhibition may offer a viable path toward extending the usefulness of β-lactam antibiotics and managing the escalating crisis of antimicrobial resistance.
Assessment of Therapeutic Potential Versus Other Novel Modalities
The escalating global health crisis of antimicrobial resistance (AMR) has positioned Methicillin-resistant Staphylococcus aureus (MRSA) as a formidable clinical challenge. This pathogen's resistance to multiple antibiotic classes, particularly β-lactams, is primarily mediated by the BlaR1 sensor receptor and the alternative penicillin-binding protein PBP2a (encoded by the mecA gene) [80] [81]. The therapeutic landscape is increasingly exploring novel modalities that extend beyond conventional antibiotics, including natural compounds, antimicrobial peptides (AMPs), and immunotherapeutic approaches [82] [83] [84]. This application note provides a structured assessment of BlaR sensor inhibitors relative to other emerging anti-MRSA strategies, offering detailed experimental frameworks for evaluating their therapeutic potential within integrated resensitization approaches.
Comparative Landscape of Anti-MRSA Therapeutic Modalities
Table 1: Quantitative Comparison of Novel Anti-MRSA Therapeutic Modalities
| Therapeutic Modality | Molecular Target(s) | Advantages | Development Stage | Key Challenges |
|---|---|---|---|---|
| BlaR Sensor Inhibitors | BlaR1 signal transduction, PBP2a expression [80] [81] | β-lactam resensitization, potential synergy with existing antibiotics [81] | Early research (in silico/preclinical) [80] | Limited candidate compounds, complex resistance regulation |
| Natural Compound Efflux Inhibitors | SAV1866 multidrug ABC transporter, MecA [82] | Multi-target engagement, diverse chemical scaffolds [82] | Computational screening with in vitro validation [82] | Optimization for bioavailability, potency verification |
| Antimicrobial Peptides (AMPs) | Bacterial membrane integrity, immunomodulation [84] | Broad-spectrum activity, low resistance development [84] | FDA-approved candidates available, clinical trials ongoing [84] | Potential toxicity, production costs, stability issues |
| Conventional Anti-MRSA Antibiotics | Various bacterial cell processes [85] | Established clinical use, known safety profiles [85] | Multiple FDA-approved options [85] | Increasing resistance, safety limitations (e.g., linezolid thrombocytopenia) [85] |
Table 2: Efficacy Profiles of Anti-MRSA Agents from Network Meta-Analysis
| Antibiotic | Bloodstream Infections (SUCRA %) | Pulmonary Infections (SUCRA %) | Skin/Soft Tissue Infections (SUCRA %) | Major Safety Concerns |
|---|---|---|---|---|
| Daptomycin | 73.0 (Most effective) [85] | - | - | - |
| Linezolid | - | 90.6 (Effectiveness) [85] | 86.3 (Effectiveness) [85] | Thrombocytopenia [85] |
| Vancomycin | - | - | - | Lower hepatotoxicity than linezolid/tigecycline [85] |
Experimental Protocols for BlaR Inhibitor Characterization
Protocol 1: Molecular Docking for BlaR Inhibitor Screening
Purpose: To computationally identify and prioritize potential BlaR sensor domain inhibitors through virtual screening.
Materials and Reagents:
- BlaR sensor domain (BlaRS) crystal structure (PDB: 1MWC)
- South African Natural Compounds Database (SANCDB) [82]
- Molecular docking software (AutoDock Vina or similar)
- High-performance computing cluster
Procedure:
- Protein Preparation: Obtain BlaRS crystal structure from Protein Data Bank. Remove native ligands and water molecules. Add polar hydrogens and assign Kollman charges.
- Binding Site Identification: Define the BlaRS active site using literature coordinates, particularly focusing on the carboxylated lysine residue essential for β-lactam binding [80] [81].
- Compound Library Preparation: Download 3D structures of natural compounds from SANCDB (https://sancdb.rubi.ru.ac.za/). Generate low-energy conformers and optimize geometries.
- Docking Parameters: Set exhaustiveness to 32, energy range to 5, and maximum poses to 20. Use grid box dimensions 25×25×25 Å centered on the active site.
- Virtual Screening: Execute batch docking against entire compound library. Record binding affinities (ΔG in kcal/mol) and intermolecular interactions.
- Hit Selection: Prioritize compounds with binding affinities <-8.0 kcal/mol and formation of key interactions with active site residues.
Validation: Include known β-lactam antibiotics as positive controls to verify docking protocol accuracy.
Protocol 2: Kinetics of BlaR Inhibition
Purpose: To quantitatively characterize the interaction kinetics between potential inhibitors and the BlaR sensor domain.
Materials and Reagents:
- Purified BlaRS protein (homogeneous preparation)
- Candidate inhibitor compounds
- β-lactam antibiotics (positive controls)
- Stopped-flow spectrophotometer
- HPLC system with UV detection
Procedure:
- Protein Acylation Assay: Incubate 10 μM BlaRS with varying concentrations (1-100 μM) of inhibitor compounds in 50 mM phosphate buffer, pH 7.0, at 25°C.
- Reaction Monitoring: Measure acylation rates using stopped-flow spectrophotometry at 240 nm (for β-lactams) or alternative wavelengths for non-β-lactam compounds.
- Kinetic Analysis: Determine microscopic rate constants (k~2~) for acylation by fitting time-dependent absorbance changes to a single exponential function.
- Deacylation Assessment: Monitor irreversible modification by measuring residual activity after 24-hour incubation using nitrocefin hydrolysis assay.
- Conformational Change Evaluation: Employ circular dichroism spectroscopy to detect secondary structure alterations upon inhibitor binding.
Data Analysis: Calculate k~2~ values and compare with β-lactam standards (literature range: 1-26 s¯¹) [80] [81]. Classify inhibitors as irreversible if deacylation rate <0.001 s¯¹.
Research Reagent Solutions
Table 3: Essential Research Reagents for BlaR-MRSA Studies
| Reagent/Category | Specific Examples | Function/Application | Source/Reference |
|---|---|---|---|
| Molecular Targets | BlaR sensor domain (BlaRS), MecA/PBP2a, SAV1866 transporter [82] [80] | Primary targets for inhibitor screening and mechanism studies | Protein Data Bank (PDB IDs: 1MWS, 2HYD) [82] |
| Natural Compound Libraries | South African Natural Compounds Database (SANCDB) [82] | Source of diverse chemical scaffolds for virtual screening | https://sancdb.rubi.ru.ac.za/ [82] |
| Reference Antibiotics | β-lactams (positive controls), linezolid, vancomycin, daptomycin [85] | Controls for resistance profiling and comparator efficacy studies | Commercial pharmaceutical standards [85] |
| Specialized Assay Systems | Surface Plasmon Resonance (SPR), stopped-flow kinetics, molecular docking platforms [82] [83] | Binding affinity measurement and interaction kinetics | Commercial instrumentation (Biacore, etc.) [83] |
Signaling Pathways and Experimental Workflows
Diagram 1: BlaR Signaling Pathway and Inhibitor Mechanism. The diagram illustrates the native BlaR signaling pathway that leads to β-lactam resistance in MRSA (upper section) and the proposed mechanism of BlaR inhibitors that block this pathway to restore antibiotic sensitivity (lower section).
Diagram 2: BlaR Inhibitor Screening Workflow. This workflow outlines the integrated computational and experimental approach for identifying and validating BlaR inhibitors, highlighting the key stages from initial screening to resensitization assessment.
Integrated Therapeutic Potential Assessment
BlaR sensor inhibitors present a distinctive therapeutic value proposition centered on resistance reversal rather than direct bactericidal activity. Their potential lies in restoring efficacy to existing β-lactam antibiotics, which boast established safety profiles and low manufacturing costs [80] [81] [86]. When benchmarked against other modalities, BlaR inhibitors occupy a complementary niche: whereas AMPs and conventional antibiotics directly target bacterial viability, BlaR inhibitors function as resistance breakers that could dramatically extend the clinical lifespan of multiple antibiotic classes.
The most promising development strategy involves combination therapies pairing BlaR inhibitors with resensitized β-lactams. This approach potentially addresses the resistance mechanisms mediated by both BlaR signaling and multidrug efflux pumps [82]. Future optimization should focus on improving inhibitor pharmacokinetics to match companion antibiotics and exploring hybrid molecules that simultaneously target BlaR and structurally related resistance elements.
BlaR sensor inhibitors represent a mechanistically distinct approach within the MRSA therapeutic landscape, with their primary value residing in resistance disruption rather than direct pathogen killing. Their development requires specialized screening methodologies and validation protocols that account for the complex signaling dynamics of β-lactam resistance. As combination therapies gain prominence in antimicrobial development, BlaR inhibitors offer a strategic pathway for revitalizing existing antibiotic arsenals against resistant pathogens. Their ultimate therapeutic potential will be determined by successful integration with complementary modalities that address the multifactorial nature of MRSA resistance.
Conclusion
Inhibiting the BlaR1 sensor protein represents a paradigm-shifting strategy to resensitize MRSA to β-lactam antibiotics, moving beyond direct bactericidal approaches to disarm the pathogen's resistance machinery. The synthesis of research across foundational mechanism, inhibitor design, optimization, and validation confirms the profound potential of this adjuvant approach, with recent studies demonstrating up to 4,096-fold potentiation of antibiotic efficacy in pre-clinical models. Future directions must focus on advancing lead compounds through clinical translation, exploring combination therapies with other resistance-breaking agents, and further elucidating the intricate regulation of the bla operon. For the research and drug development community, BlaR1 inhibition offers a robust and promising framework to expand the antimicrobial arsenal and confront the escalating crisis of multidrug-resistant bacterial infections.
References
- 1. Activation of BlaR1 Protein of Methicillin-resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3207446/]
- 2. Binding of the Gene Repressor BlaI to the bla Operon in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2942778/]
- 3. Structural basis of broad-spectrum β-lactam resistance in ... [https://www.nature.com/articles/s41586-022-05583-3]
- 4. An experiment-informed signal transduction model for the ... [https://www.nature.com/articles/s41598-019-55923-z]
- 5. Phosphorylation of BlaR1 in Manifestation of Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5022795/]
- 6. Activation of BlaR1 Protein of Methicillin-resistant ... [https://www.sciencedirect.com/science/article/pii/S0021925820506583]
- 7. Crystal Structures of the BlaI Repressor from Staphylococcus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1064009/]
- 8. Investigation of Signal Transduction Routes within the Sensor/Transducer Protein BlaR1 of Staphylococcus aureus - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4691190/]
- 9. Researchers pinpoint mechanism responsible for MRSA's ... [https://www.dental.umaryland.edu/about/news/february-2023/researchers-pinpoint-mechanism-responsible-for-mrsas-resistance-to-antibiotics.php]
- 10. Structural basis of broad-spectrum β-lactam resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9834060/]
- 11. Activation of BlaR1 Protein of Methicillin-resistant Staphylococcus aureus, Its Proteolytic Processing, and Recovery from Induction of Resistance - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3207446/]
- 12. Structural analysis of avibactam-mediated activation of the ... [https://www.sciencedirect.com/science/article/pii/S0021925817491915]
- 13. Mechanisms and functions of protein S-acylation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010433/]
- 14. Protein acylation: mechanisms, biological functions and ... [https://www.nature.com/articles/s41392-022-01245-y]
- 15. Restoring susceptibility to β-lactam antibiotics in methicillin ... [https://pubmed.ncbi.nlm.nih.gov/39060390/]
- 16. The function and mechanism of protein acylation in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279274/]
- 17. Targeted inhibition of mecA and agrA genes in clinical ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1643774/full]
- 18. Molecular Determinants of β-Lactam Resistance in ... [https://www.mdpi.com/2079-6382/12/9/1362]
- 19. A gratuitous β-Lactamase inducer uncovers hidden active site ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197241]
- 20. Co-blockade of mecR1/blaR1 signal pathway to restore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3258742/]
- 21. Unmasking MRSA's Armor: Molecular Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388575/]
- 22. Molecular Determinants of β-Lactam Resistance in Methicillin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10525618/]
- 23. Phosphorylation of BlaR1 in Manifestation of ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/27623311/]
- 24. Structure-Function Studies of the Staphylococcal Methicillin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3774396/]
- 25. Discovery of Boronic Acids-Based β-Lactamase Inhibitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071365/]
- 26. Investigation of Signal Transduction Routes within the Sensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4691190/]
- 27. Researchers demonstrate antibiotic sensing event central ... [https://www.sciencedaily.com/releases/2011/09/110915114007.htm]
- 28. Targeting MRSA penicillin-binding protein 2a [https://www.sciencedirect.com/science/article/pii/S0006295225003132]
- 29. A gratuitous β-Lactamase inducer uncovers hidden active site ... [https://pubmed.ncbi.nlm.nih.gov/29771929/]
- 30. High-throughput analysis system of interaction kinetics for ... [https://www.nature.com/articles/s41598-023-46756-y]
- 31. Crystal structures of the Apo and penicillin-acylated forms ... [https://pubmed.ncbi.nlm.nih.gov/15322076/]
- 32. Boronic Acids and Their Derivatives in Medicinal Chemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC7571202/]
- 33. Click Chemistry in Lead Optimization of Boronic Acids as β- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5744665/]
- 34. Boronic Acid-substituted Benzimidazole Derivatives and [https://link.springer.com/content/pdf/10.1007/s40242-025-5040-x.pdf]
- 35. Discovery and Structure-Based Optimization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8314423/]
- 36. 10058-F4 Mediated inhibition of the biofilm formation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12302182/]
- 37. The current role and evolution of X-ray crystallography in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10620067/?tool=pmcentrez]
- 38. Discovery of Novel Antimicrobial-Active Compounds and ... [https://www.mdpi.com/1420-3049/30/7/1477]
- 39. Innovative Strategies in X-ray Crystallography for Exploring Structural Dynamics and Reaction Mechanisms in Metabolic Disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11432794/]
- 40. Quantitative Analysis by XRD [https://h-and-m-analytical.com/quantitative-analysis-by-xrd/]
- 41. Engineered exosomes as drug and RNA co-delivery system [https://pmc.ncbi.nlm.nih.gov/articles/PMC10562639/]
- 42. Bio fluid exosomes: promises, challenges, and future ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06886-5]
- 43. Exosomes in cancer nanomedicine - Molecular Cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02372-0]
- 44. siRNA-AGO2 complex inhibits bacterial gene translation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11970400/]
- 45. A comprehensive review on recent advances in exosome ... [https://www.sciencedirect.com/science/article/pii/S1936523324002481]
- 46. Qualitative and Quantitative Comparison of Plasma Exosomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919666/]
- 47. Role of β-Lactamase Inhibitors as Potentiators in Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10967447/]
- 48. New β-Lactam/β-Lactamase Inhibitor Combination Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029989/]
- 49. β-Lactam potentiators to re-sensitize resistant pathogens [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1092556/full]
- 50. Antibiotic potentiators as a promising strategy for ... [https://www.nature.com/articles/s44259-025-00112-4]
- 51. Overcoming the drug resistance barrier: progress in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1702881/full]
- 52. Lysine Nζ-Decarboxylation Switch and Activation of the β ... [https://www.sciencedirect.com/science/article/pii/S0021925820722568]
- 53. Promising Future of Novel Beta-Lactam Antibiotics Against ... [https://pubmed.ncbi.nlm.nih.gov/41090025/]
- 54. Crystal Structures of the Apo and Penicillin-acylated Forms ... [https://www.sciencedirect.com/science/article/pii/S0021925820699525]
- 55. Drug Repurposing: An Emerging Strategy in Staphylococcus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603381/]
- 56. Benzoxaboroles in medicinal chemistry: A structure-guided ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425009894]
- 57. UNC2025, a Potent and Orally Bioavailable MER/FLT3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4148167/]
- 58. Structural analysis of avibactam-mediated activation of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7415986/]
- 59. Fighting Methicillin-Resistant Staphylococcus aureus with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10219003/]
- 60. Stimuli-responsive nanocarriers for drug delivery, tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7150471/]
- 61. Stimuli-responsive nanocarriers for therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8185873/]
- 62. Advances in stimuli-responsive nanoparticles for cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725009220]
- 63. Honokiol-loaded nanoparticles for targeted bacterial ... [https://www.sciencedirect.com/science/article/pii/S2590006425011330]
- 64. Using generative AI, researchers design compounds that ... [https://news.mit.edu/2025/using-generative-ai-researchers-design-compounds-kill-drug-resistant-bacteria-0814]
- 65. Disarming Staphylococcus aureus: Review of Strategies ... [https://www.mdpi.com/2076-0817/14/4/386]
- 66. Scientists turn superbug MRSA into treatable infection [https://www.drugtargetreview.com/news/157354/scientists-turn-superbug-mrsa-into-treatable-infection/]
- 67. Synergistic cefiderocol-containing antibiotic combinations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494139/]
- 68. Synergistic combinations of antimicrobial peptides and ... [https://www.sciencedirect.com/science/article/pii/S0031699725075131]
- 69. The Importance of Murine Models in Determining In Vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944934/]
- 70. A step forward on the in vitro and in vivo validation of ... [https://www.sciencedirect.com/science/article/pii/S0168365925000938]
- 71. A Model for Evaluating Topical Antimicrobial Efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3421576/]
- 72. Targeting MRSA penicillin-binding protein 2a [https://pubmed.ncbi.nlm.nih.gov/40484039/]
- 73. A strategic approach to overcome resistance in MRSA [https://www.sciencedirect.com/science/article/abs/pii/S0968089625000744]
- 74. Unraveling the mechanism of ceftaroline-induced allosteric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10720500/]
- 75. The Quinazolinone Allosteric Inhibitor of PBP 2a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6496080/]
- 76. Designing Novel Nucleoside Inhibitors the Targeting Site... Allosteric [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5029716]
- 77. Methicillin-Resistant Staphylococcus aureus (MRSA) [https://www.mdpi.com/2079-6382/14/8/771]
- 78. Novel strategy to reduce antibiotic resistance in a superbug [https://lightsources.org/2025/04/02/novel-strategy-to-reduce-antibiotic-resistance-in-a-superbug/]
- 79. Natural Inhibitors from Ganoderma lucidum Targeting ... [https://journal.uny.ac.id/publications/jomassh/article/view/1144]
- 80. Resistance to beta-lactam antibiotics and its ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/12591921/]
- 81. Resistance to β-Lactam Antibiotics and Its Mediation by the ... [https://www.sciencedirect.com/science/article/pii/S0021925819549456]
- 82. Potential Natural Inhibitors of MRSA ABC Transporters and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195973/]
- 83. Evolution of preclinical characterization and insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9372426/]
- 84. Antimicrobial Peptides: The Game-Changer in the Epic ... [https://www.mdpi.com/1424-8247/17/11/1555]
- 85. Comparative effectiveness and safety of six antibiotics in ... [https://pubmed.ncbi.nlm.nih.gov/38789000/]
- 86. β-Lactamases and β-Lactamase Inhibitors in the 21st Century [https://pmc.ncbi.nlm.nih.gov/articles/PMC6723624/]